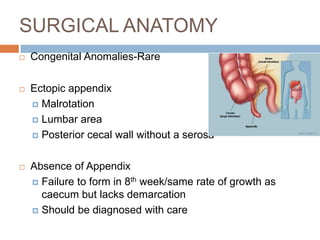
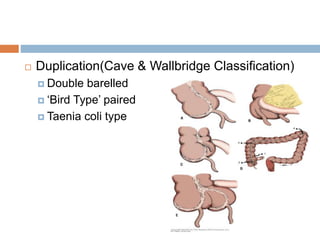
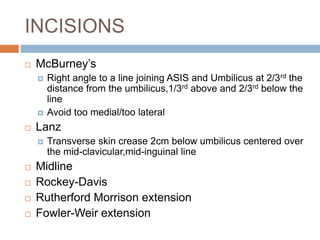
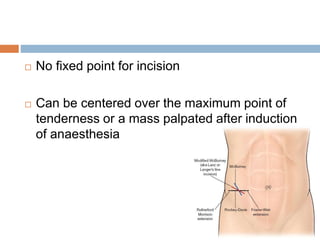
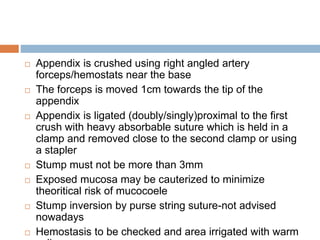
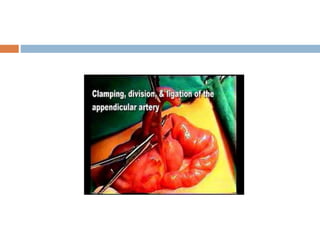
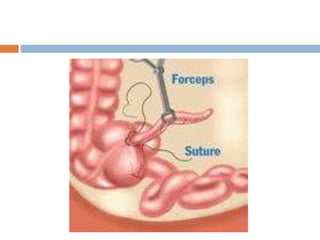
This document outlines the steps in an open appendectomy procedure. It begins with a description of surgical anatomy including variations such as ectopic or absent appendix. It then discusses pre-operative preparation, incision sites, and identification of the appendix. The key steps are: delivering the cecum into the wound, identifying the appendix base, applying clamps and removing the appendix from tip to base while ligating vessels. The appendix is then ligated and the stump may be cauterized before closing tissue layers and applying dressings. Variations for complicated cases are also noted.