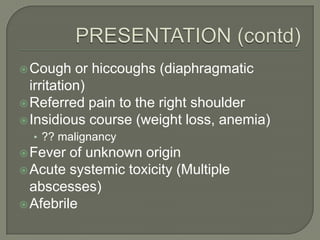
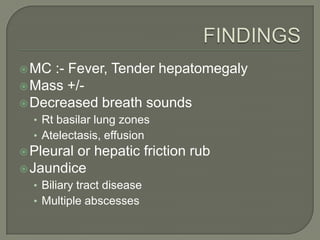
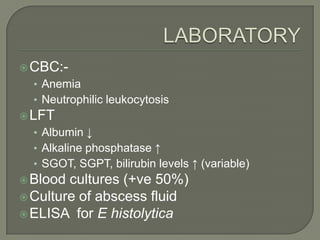
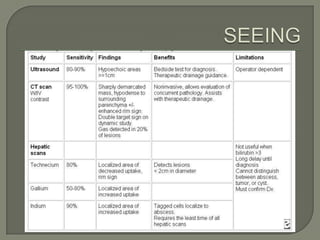
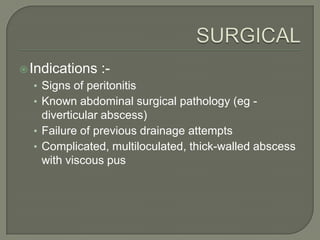
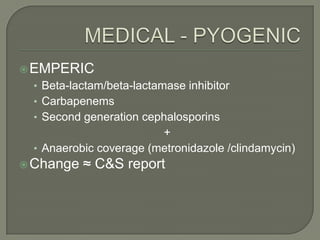
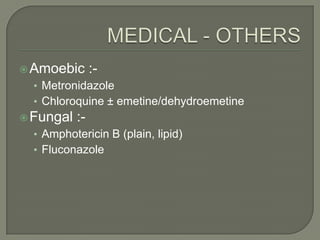
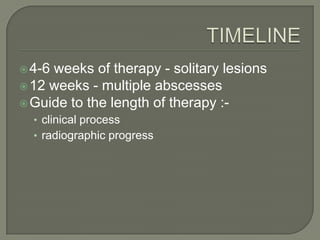
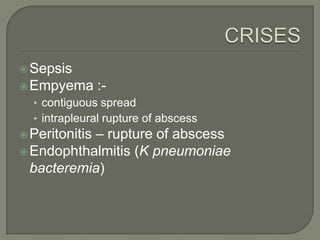
Liver abscesses are relatively rare but mortality has decreased to 5-30% due to improved diagnostic and treatment methods. Risk factors include diabetes, liver transplants, and immunosuppression. Symptoms include fever, right upper quadrant pain, and referred shoulder pain. Diagnosis involves blood tests, imaging like CT or ultrasound, and abscess drainage or long-term antibiotic therapy. Complications can include sepsis, empyema, or peritonitis if left untreated. Prognosis is worse with multiple abscesses, underlying illnesses, or delays in diagnosis and treatment.