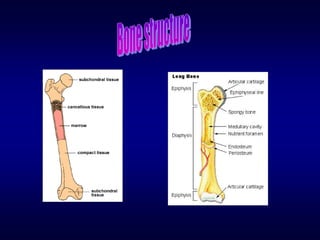
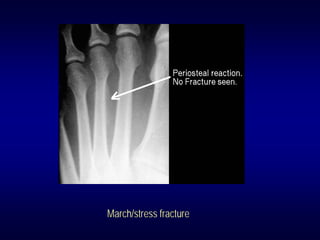
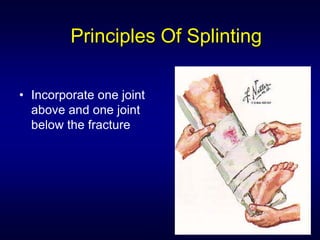
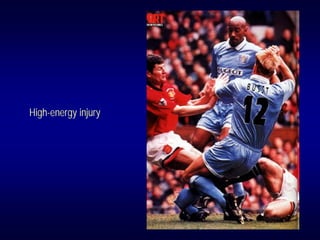
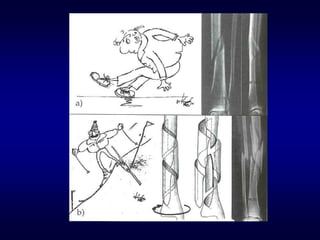
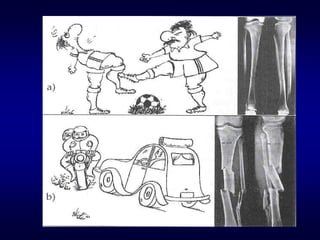
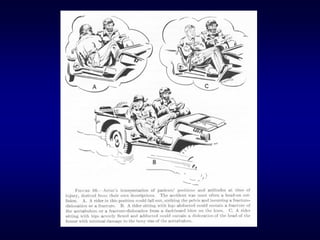
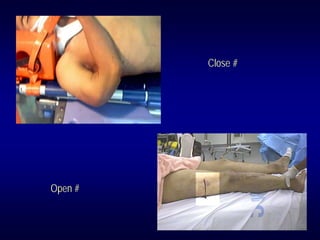
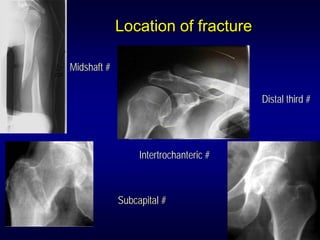
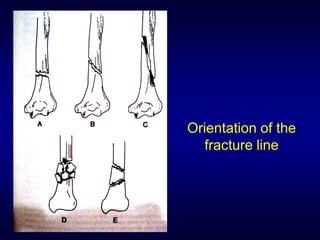
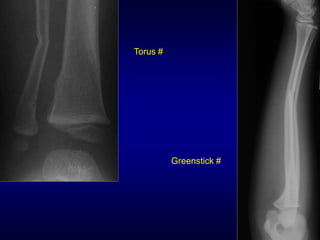
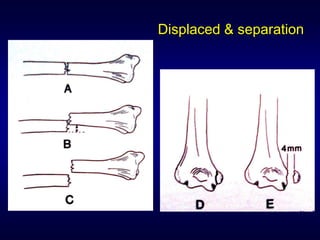
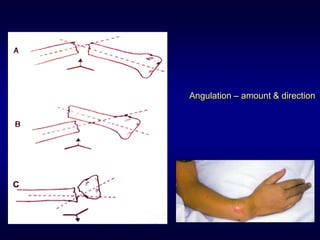
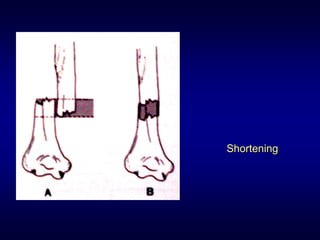
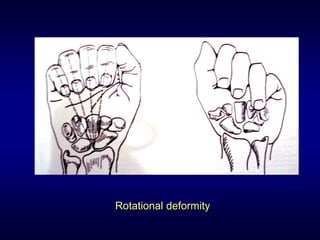
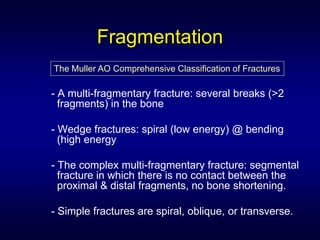
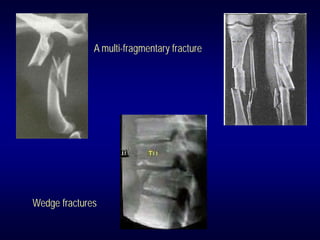
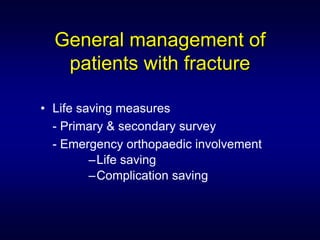
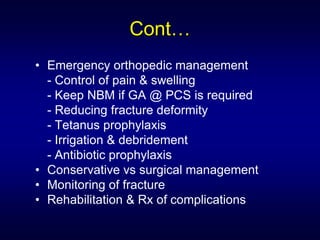
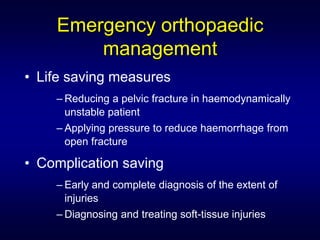
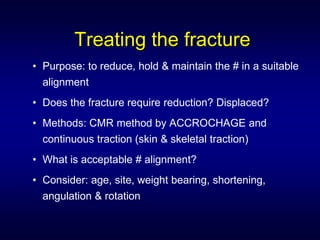
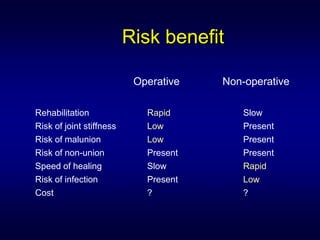
This document provides an overview of fracture care. It discusses understanding fractures, describing fractures based on clinical and radiological features, and principles of fracture management. Key points include: fractures disrupt bone integrity; they occur through typical, pathologic, or stress mechanisms; goals of treatment are to restore function, prevent complications, and allow healing; and prehospital care involves splinting and transporting the patient for further evaluation and treatment.