1) Casting is used to immobilize fractures and correct deformities by applying uniform pressure.
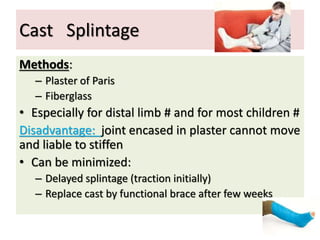
2) Plaster of Paris and fiberglass are common casting materials, with fiberglass preferred for distal limbs and children due to its lighter weight.
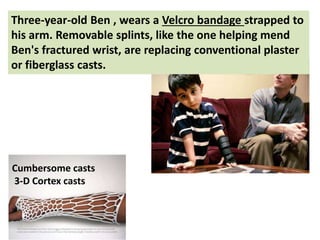
3) Ben, a 3-year old, wore a removable splint instead of a conventional cast to mend his fractured wrist, as removable splints are replacing casts.