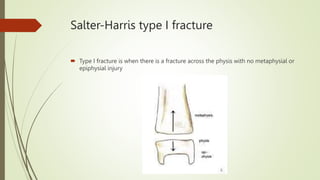
Fractures are breaks in bone continuity that can range from complete breaks to incomplete breaks. Globally in 2000, there were an estimated 9 million new fragility fractures, including over 1.6 million at the hip. Fractures are classified based on their anatomic features such as type, comminution, location, and displacement. Other classifications include the AO classification system for long bones, Salter-Harris classification for pediatric physeal fractures, and the Gustillo-Anderson classification for open fractures. Clinical presentation of fractures involves symptoms of pain, swelling, deformity, and loss of function as well as signs found on examination and imaging studies. Management principles involve stabilization, reduction, fixation, exercise, and physiotherapy.