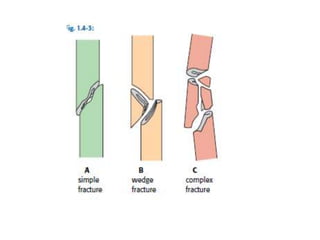
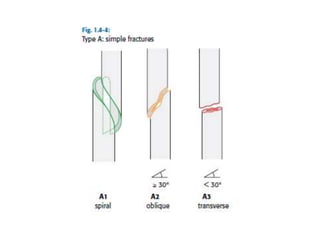
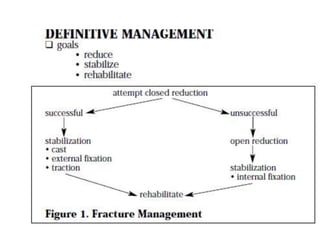
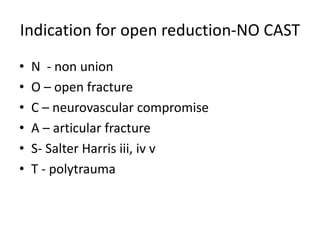
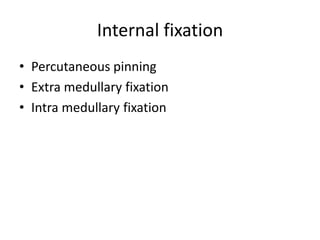
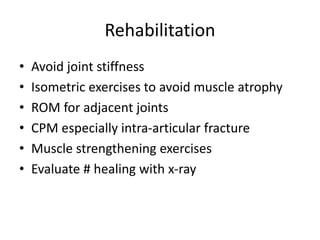
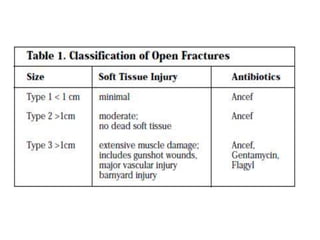
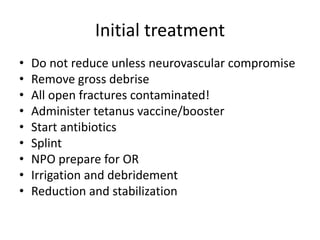
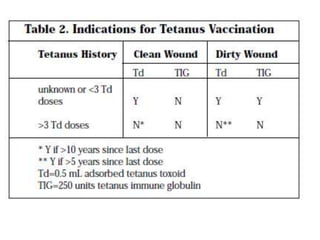
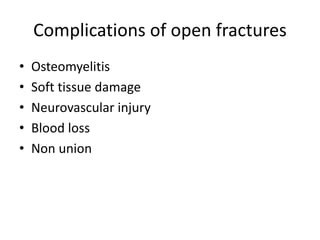
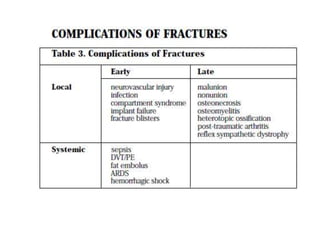
This document discusses the basic principles of fracture management. It begins by describing the case of a man found injured on the road after being hit by a vehicle. It then defines a fracture and outlines the key steps in identifying and initially managing fractures, including assessing life threats, identifying specific injuries, providing emergency treatment, and obtaining a history. It discusses fracture mechanisms and clinical features. The document emphasizes the importance of initial stabilization, splinting, analgesia, and obtaining x-rays before and after reduction. It describes indications for open versus closed reduction and different stabilization methods. Finally, it covers rehabilitation, the emergency treatment of open fractures, and potential complications.