1. Fracture is a break in the structural continuity of bone that can be caused by trauma or pathology. Fractures are classified based on etiology, communication, and shape.
2. Evaluation of fractures involves history, physical exam, and imaging studies like x-rays. Treatment depends on the fracture type but generally involves reduction, immobilization, and rehabilitation.
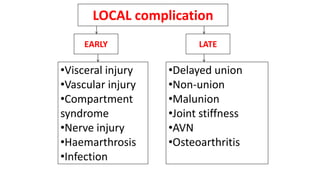
3. Complications of fractures include infection, malunion, nonunion, and impaired function. Open fractures require emergent irrigation, debridement, and antibiotic treatment to prevent infection.