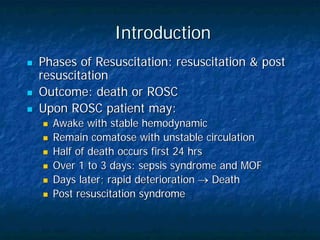
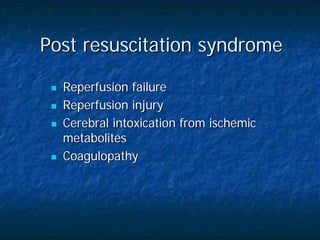
The document outlines the importance of post resuscitation care to stabilize patients after return of spontaneous circulation, including supporting oxygenation and circulation, treating injuries from CPR, monitoring for recurrent cardiac arrest, and promptly transferring patients to intensive care units for specialized monitoring and treatment. Proper post resuscitation care is critical to optimize outcomes in the hours after resuscitation.