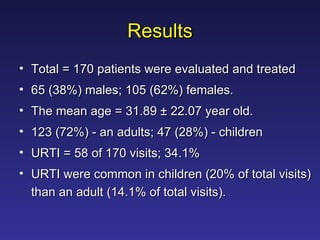
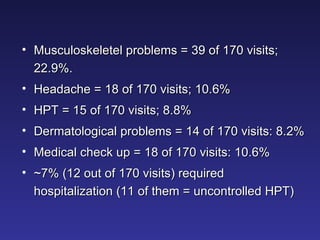
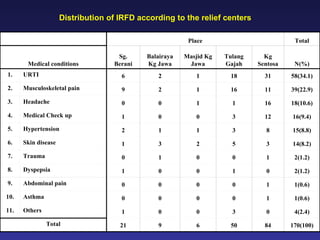
The document summarizes a study on illnesses related to flood disasters at relief centers in Malaysia. It found that the most common illnesses were upper respiratory tract infections (URTI), musculoskeletal pain, headaches, and uncontrolled hypertension. URTI was likely due to overcrowding and difficulties maintaining hygiene. Musculoskeletal pain resulted from rescue efforts during the flood. Headaches were caused by stress and disrupted medical infrastructure led to uncontrolled hypertension. Overall, the study aimed to help medical relief teams prepare for future flood disasters.