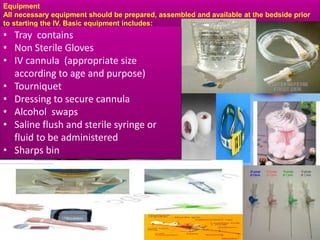
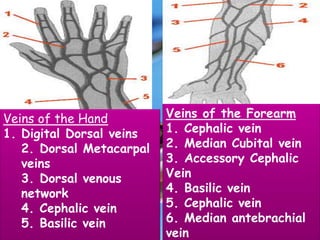
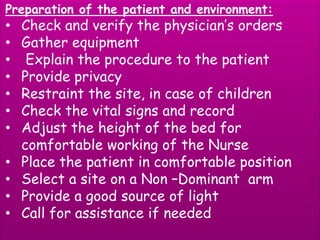
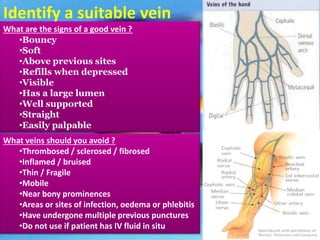
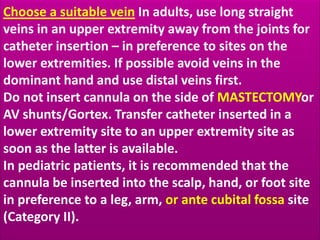
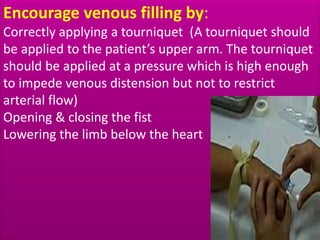
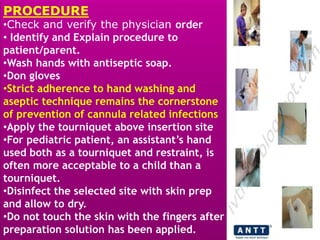
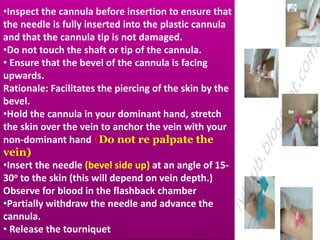
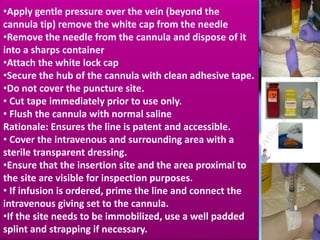
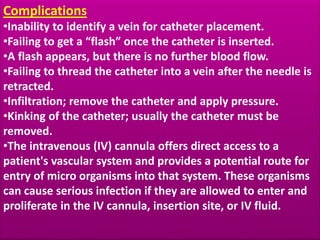
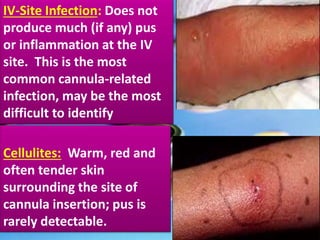
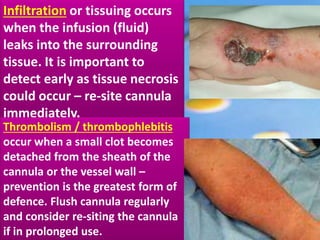
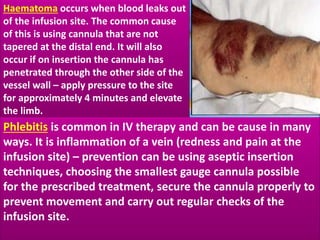
This document provides guidance on inserting a peripheral intravenous cannula. It describes the equipment needed, vein selection, insertion procedure, documentation, and potential complications. The aim is to safely deliver treatment without discomfort or tissue damage while maintaining venous access. Proper preparation, aseptic technique, and site care are emphasized to prevent infections and other complications.