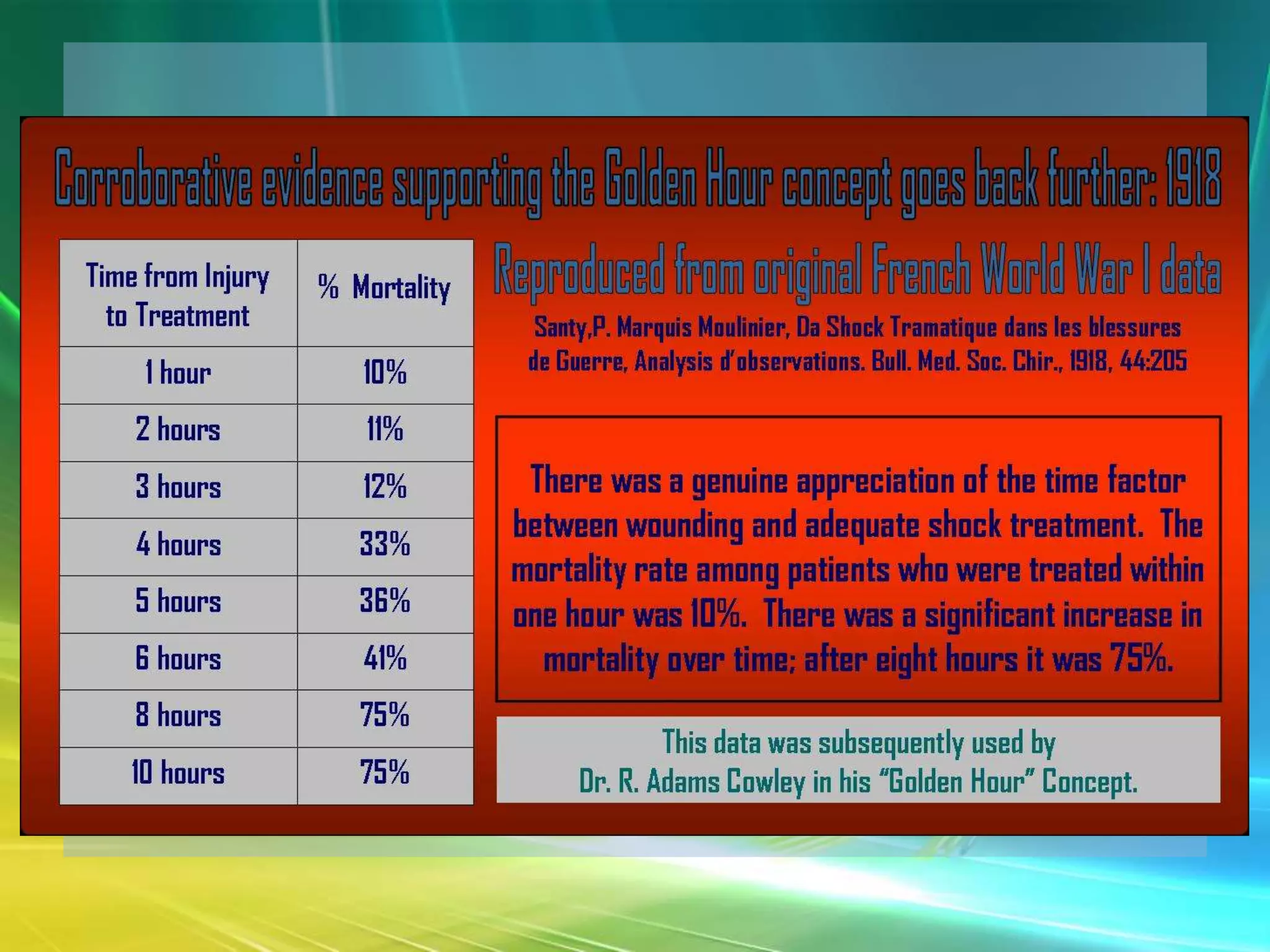
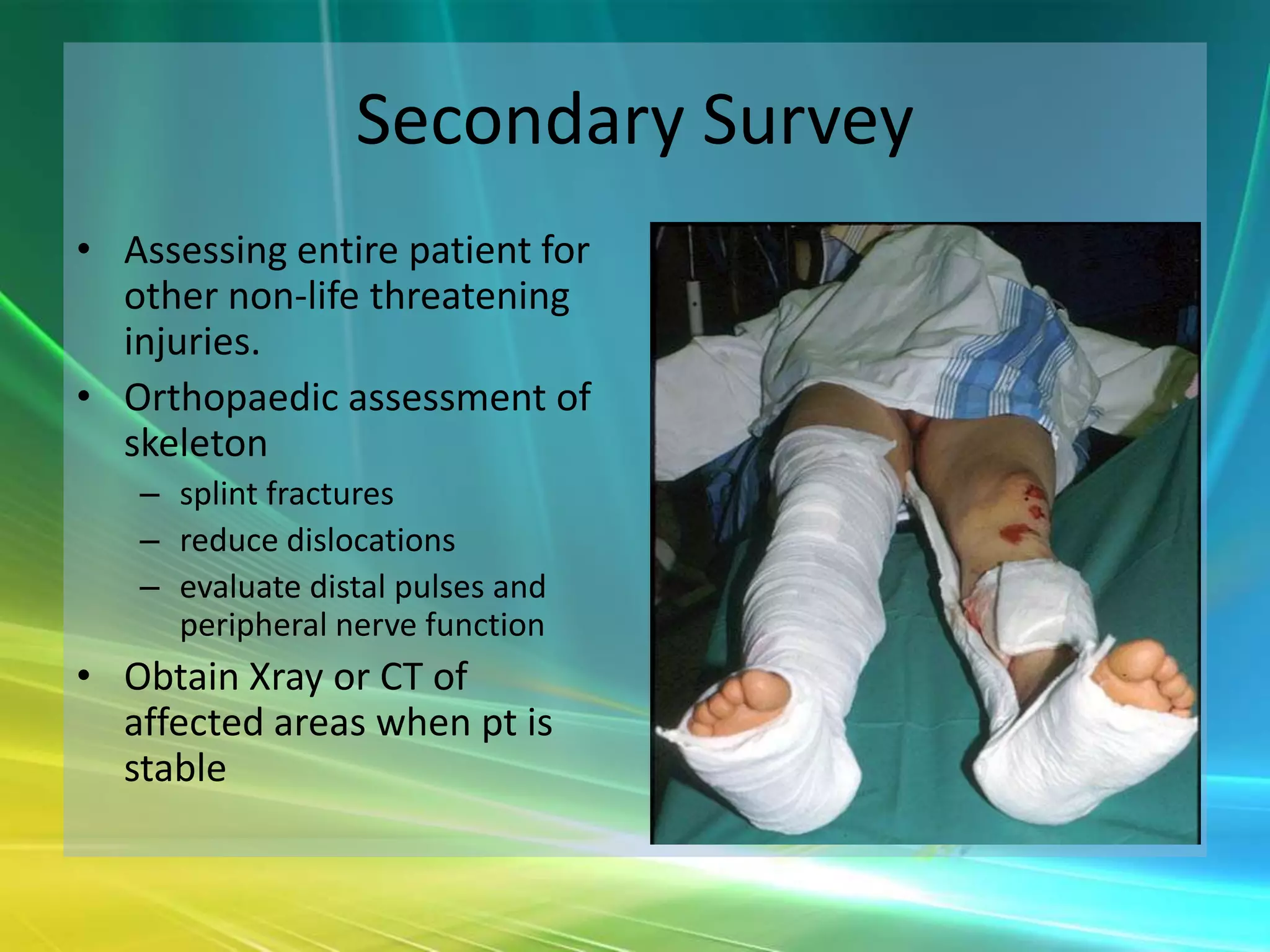
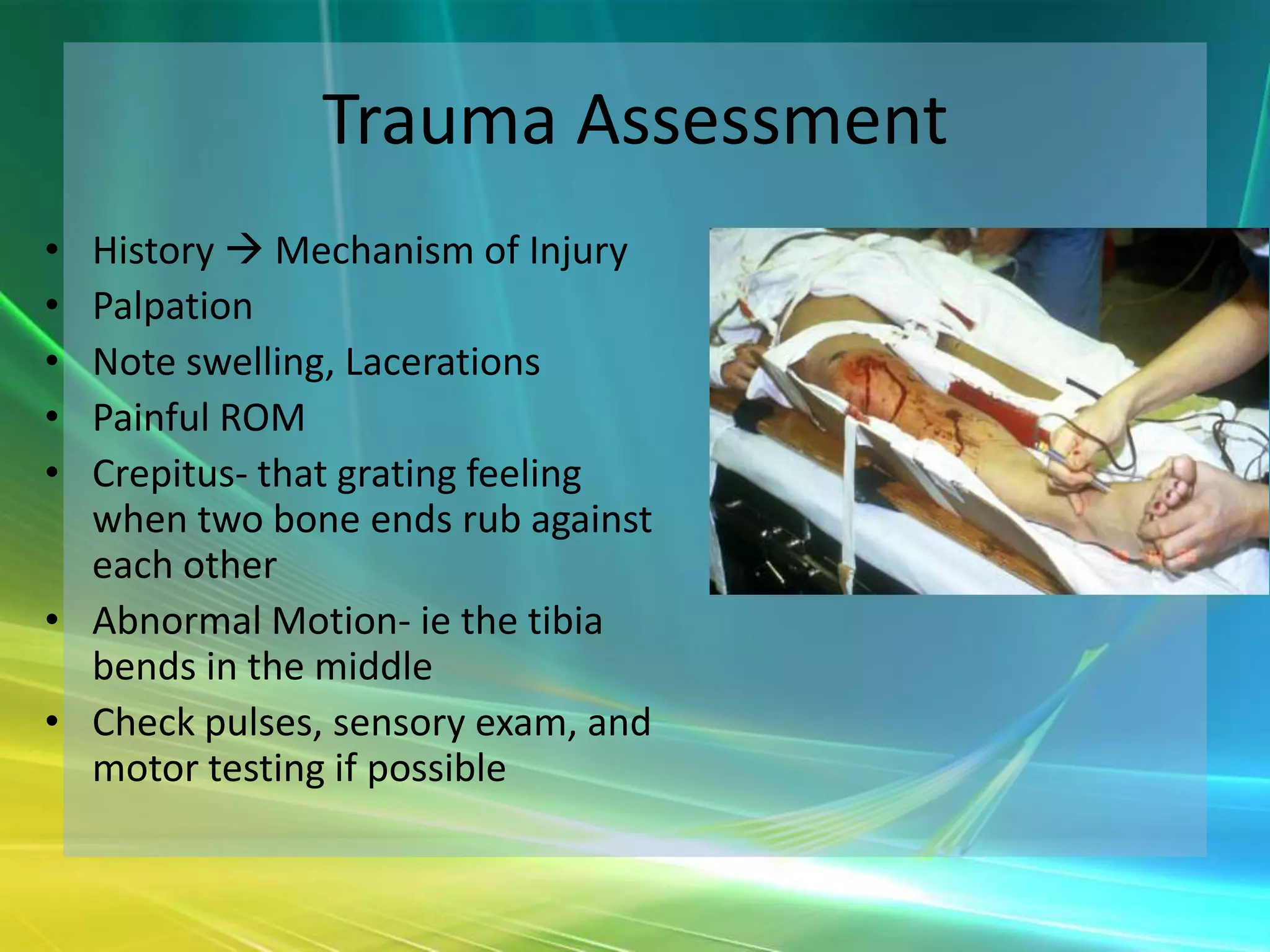
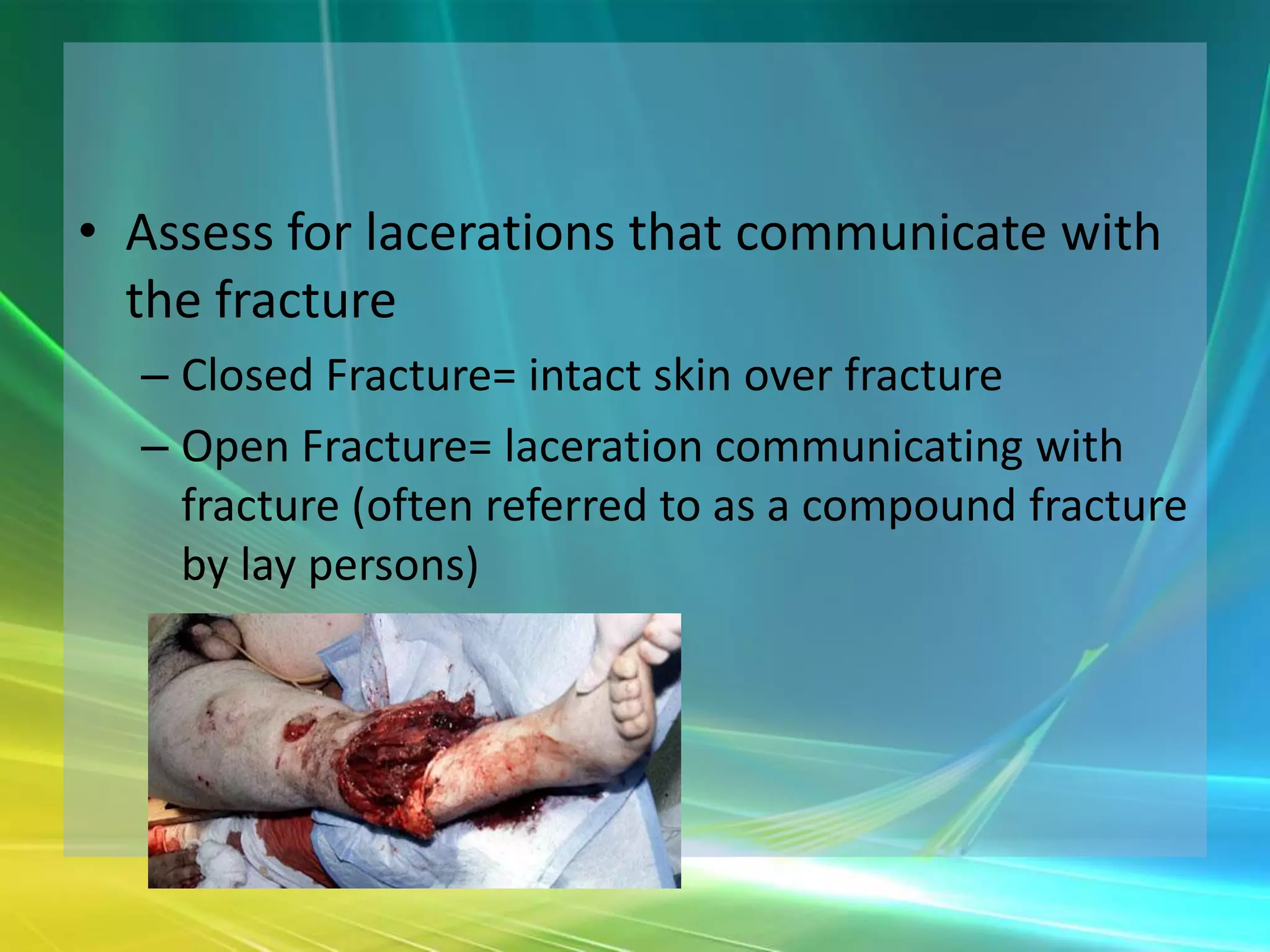
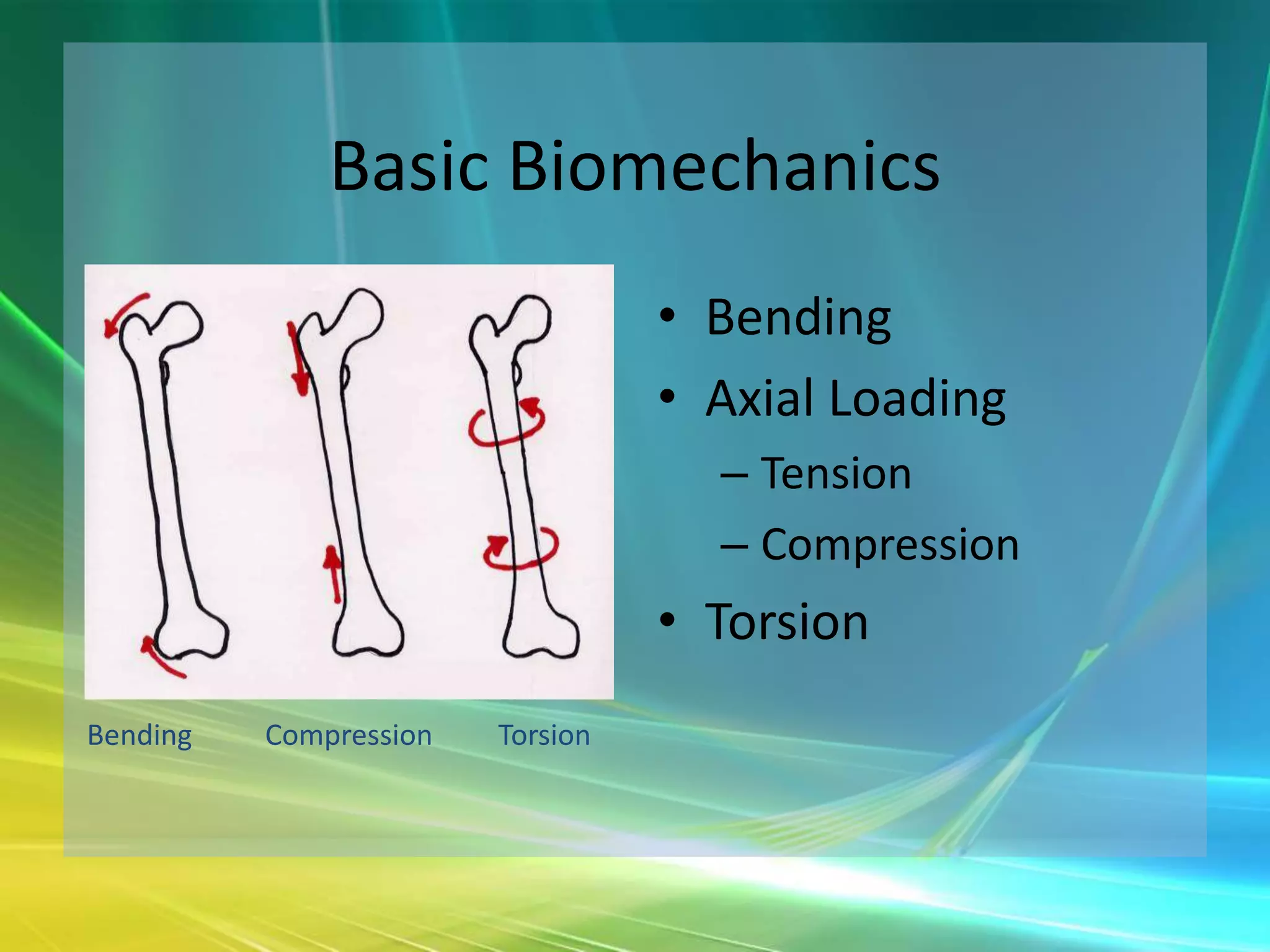
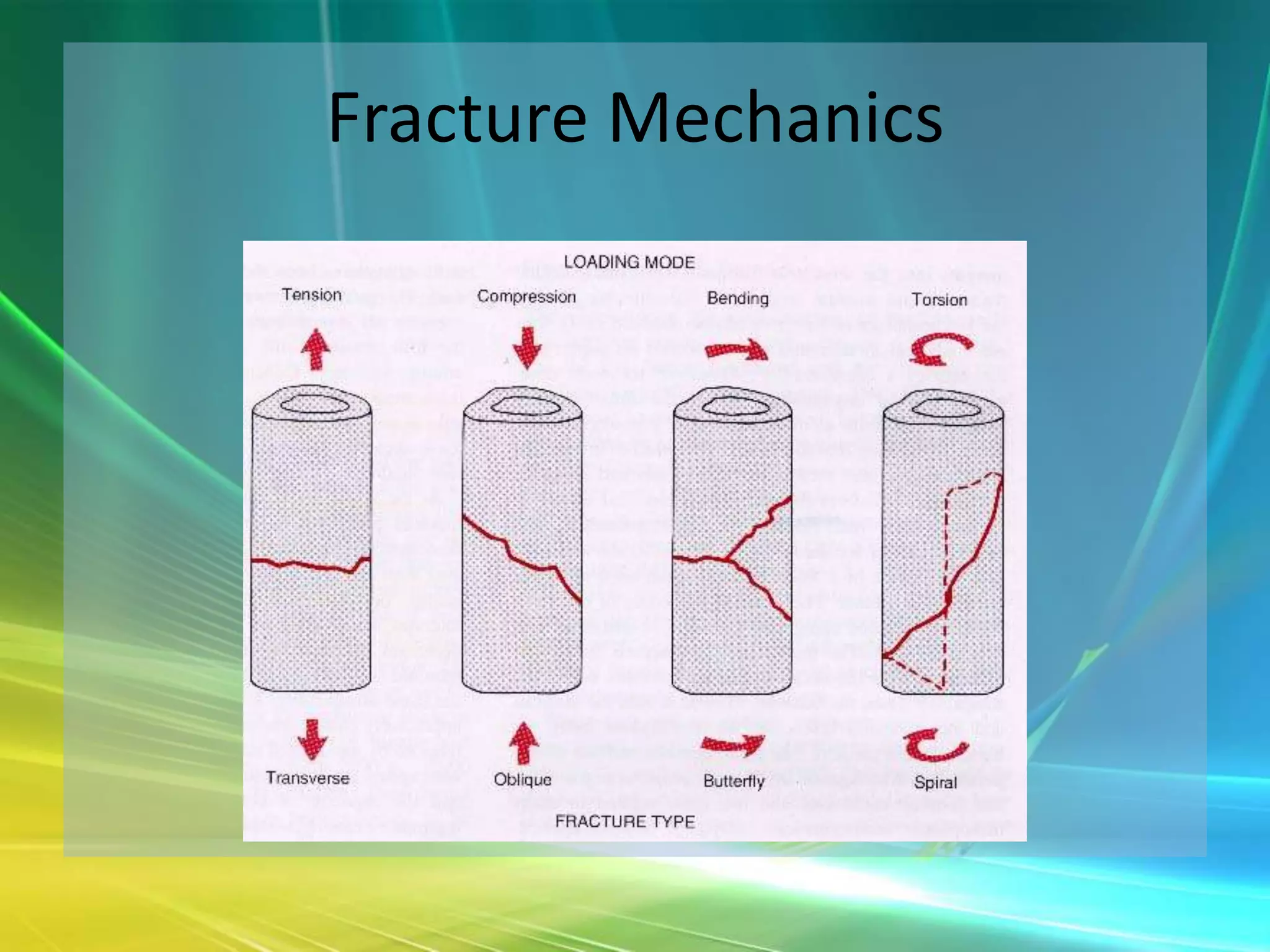
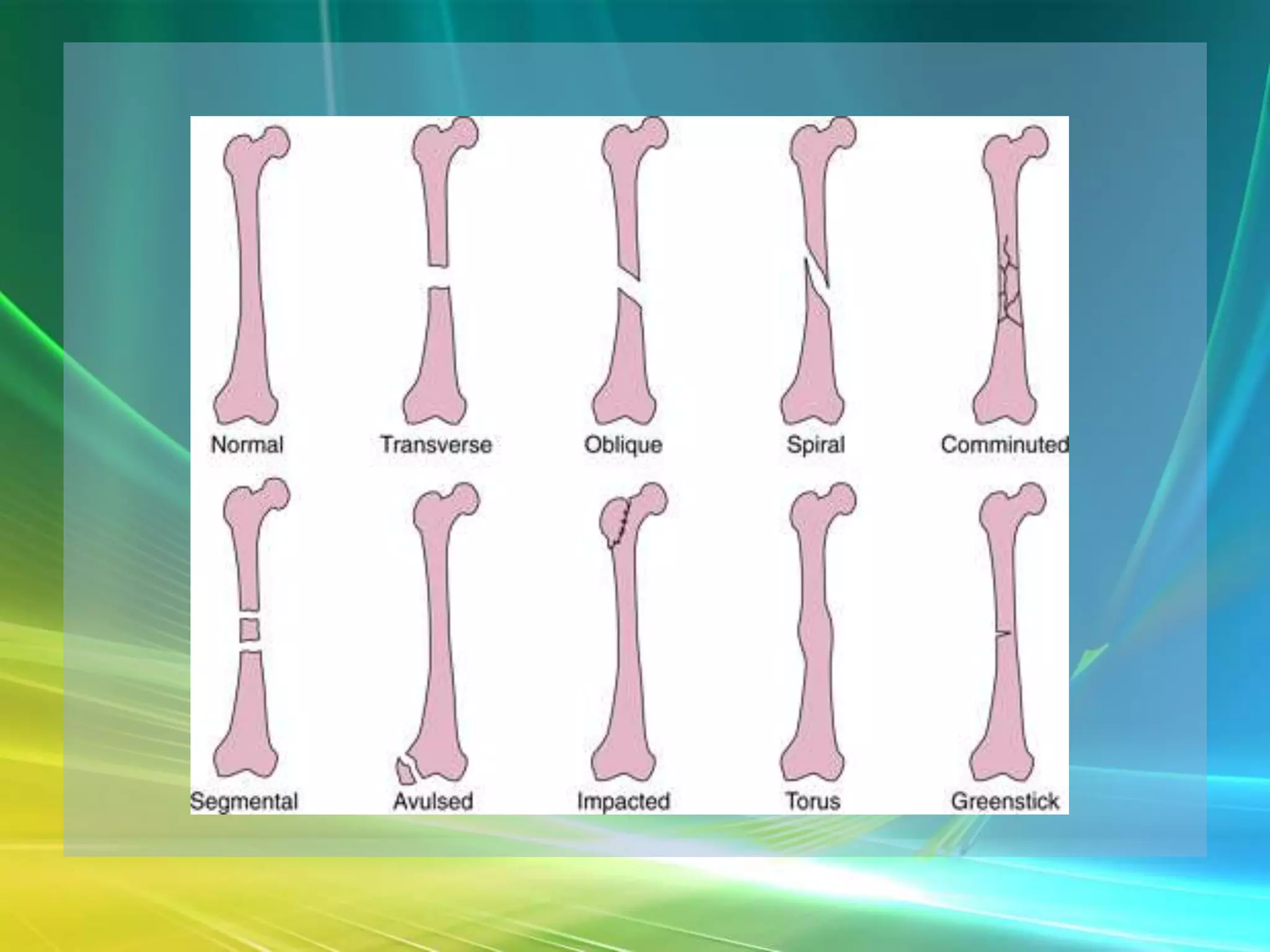
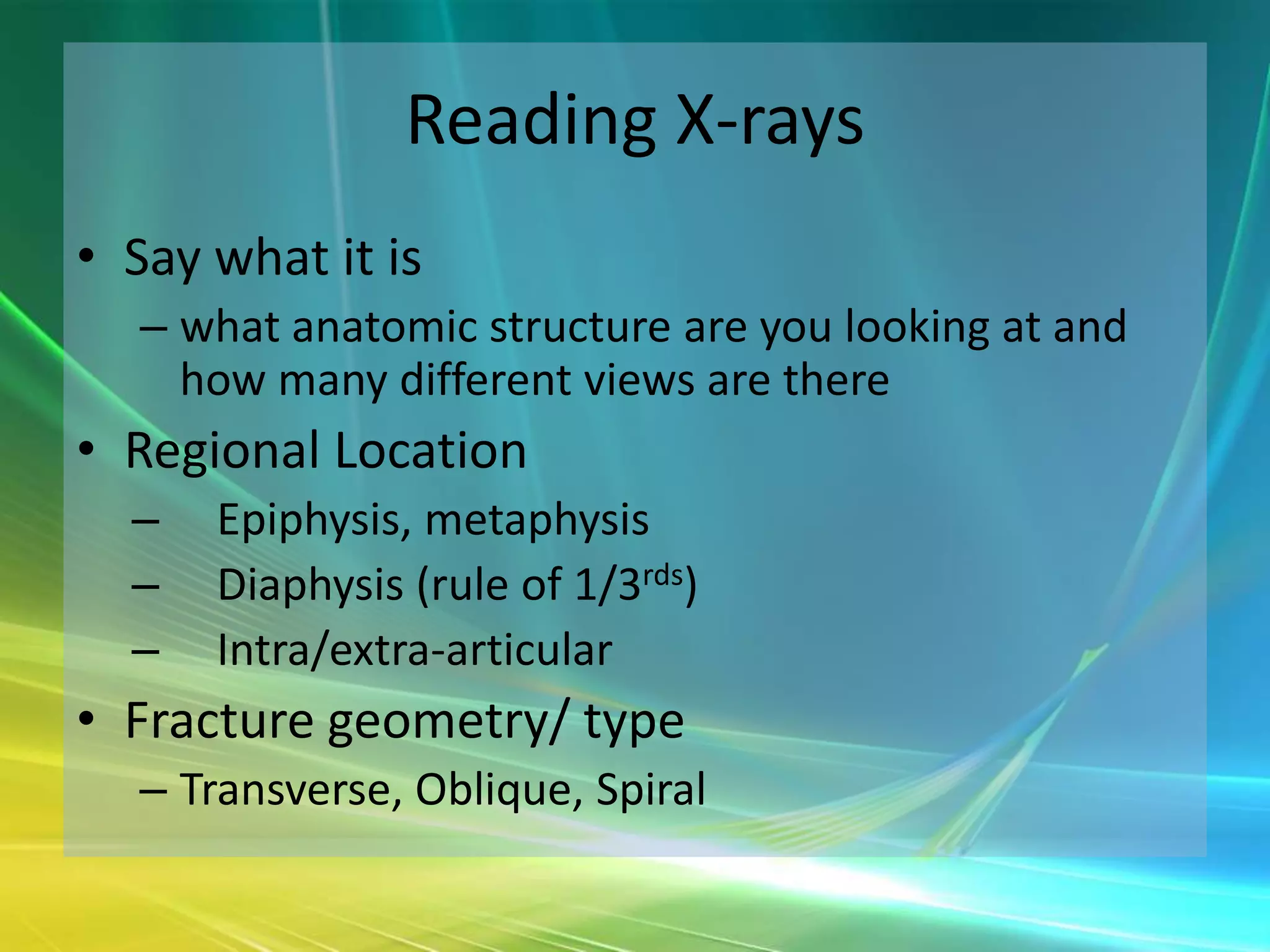
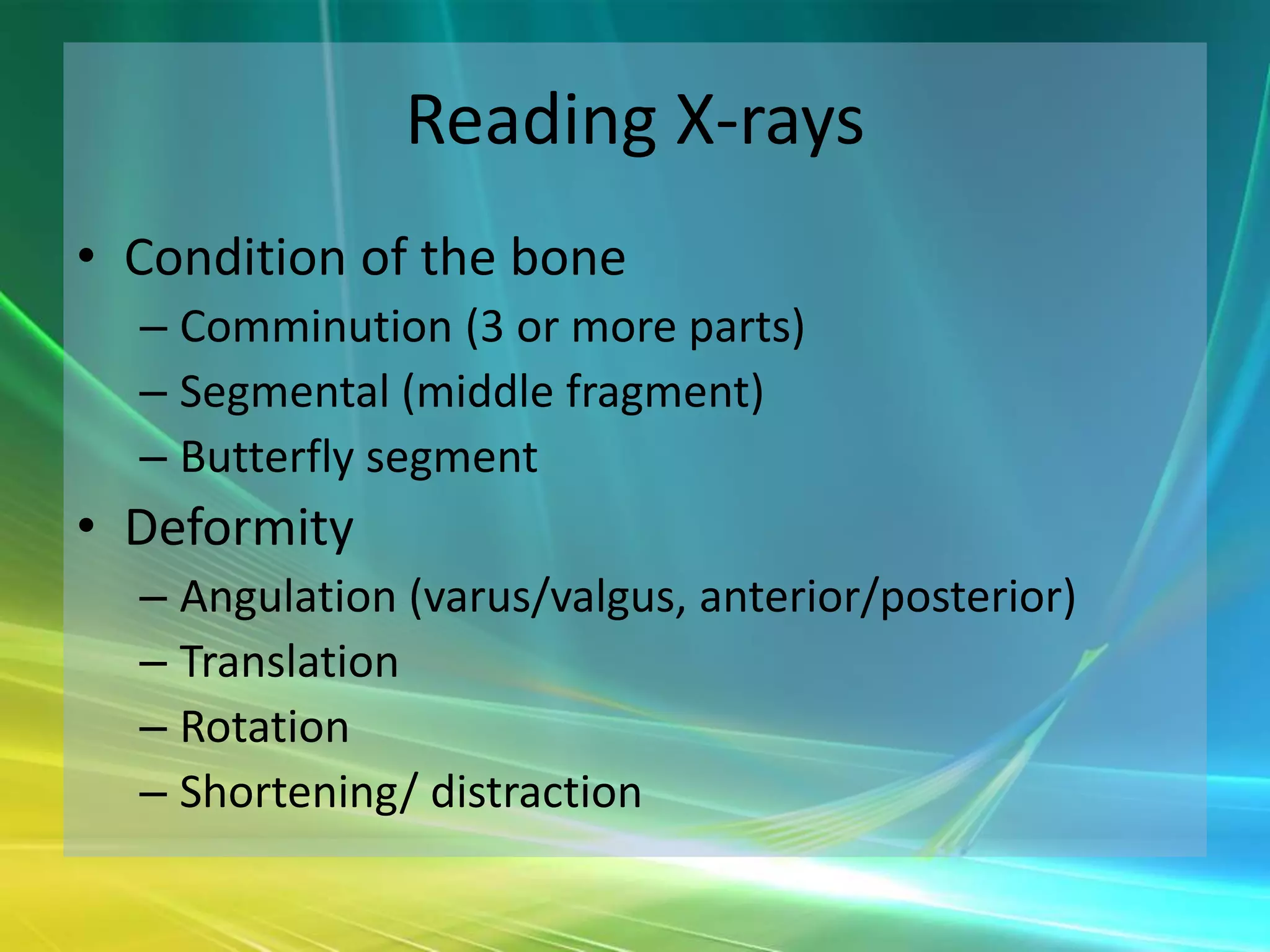
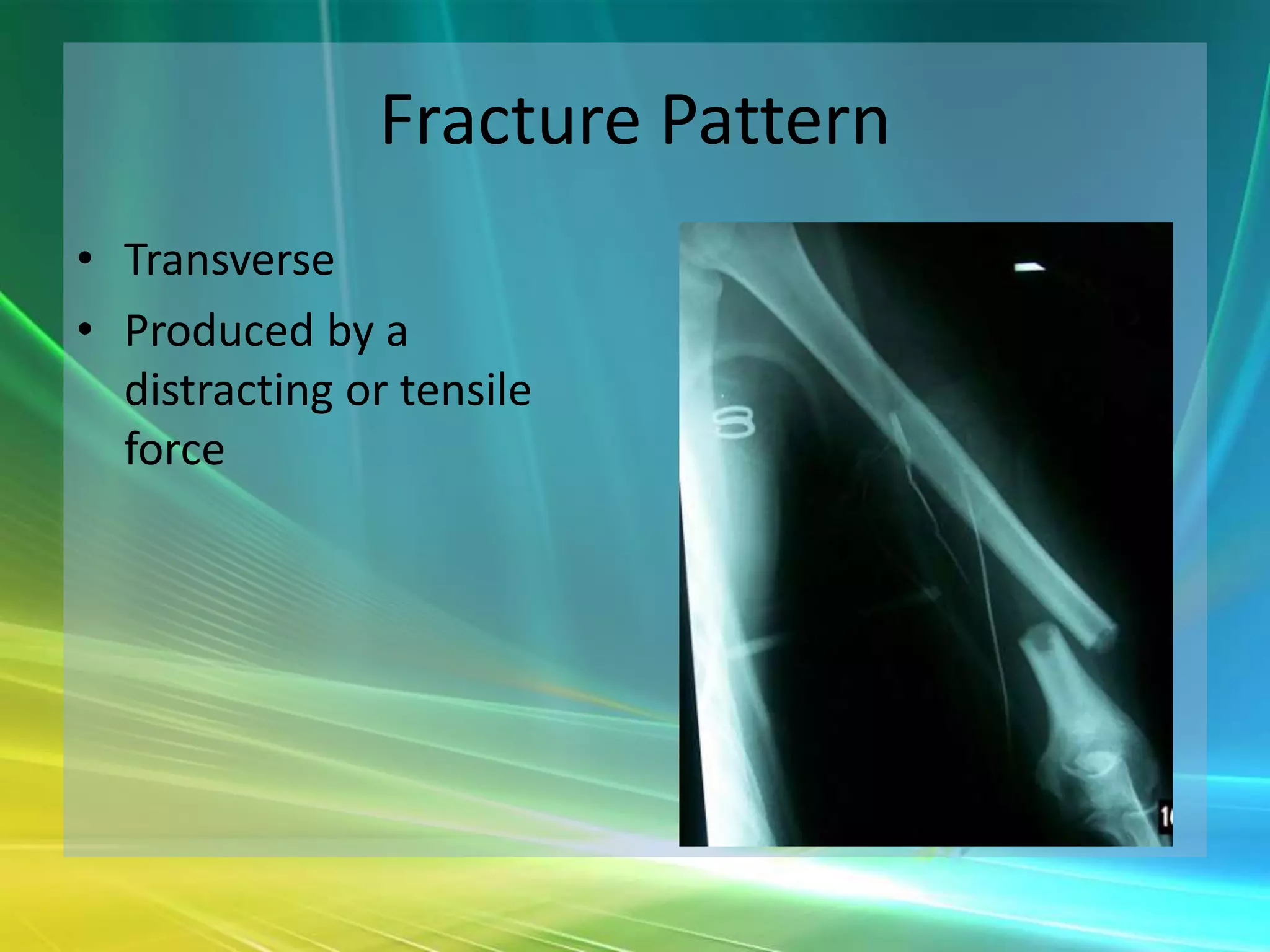
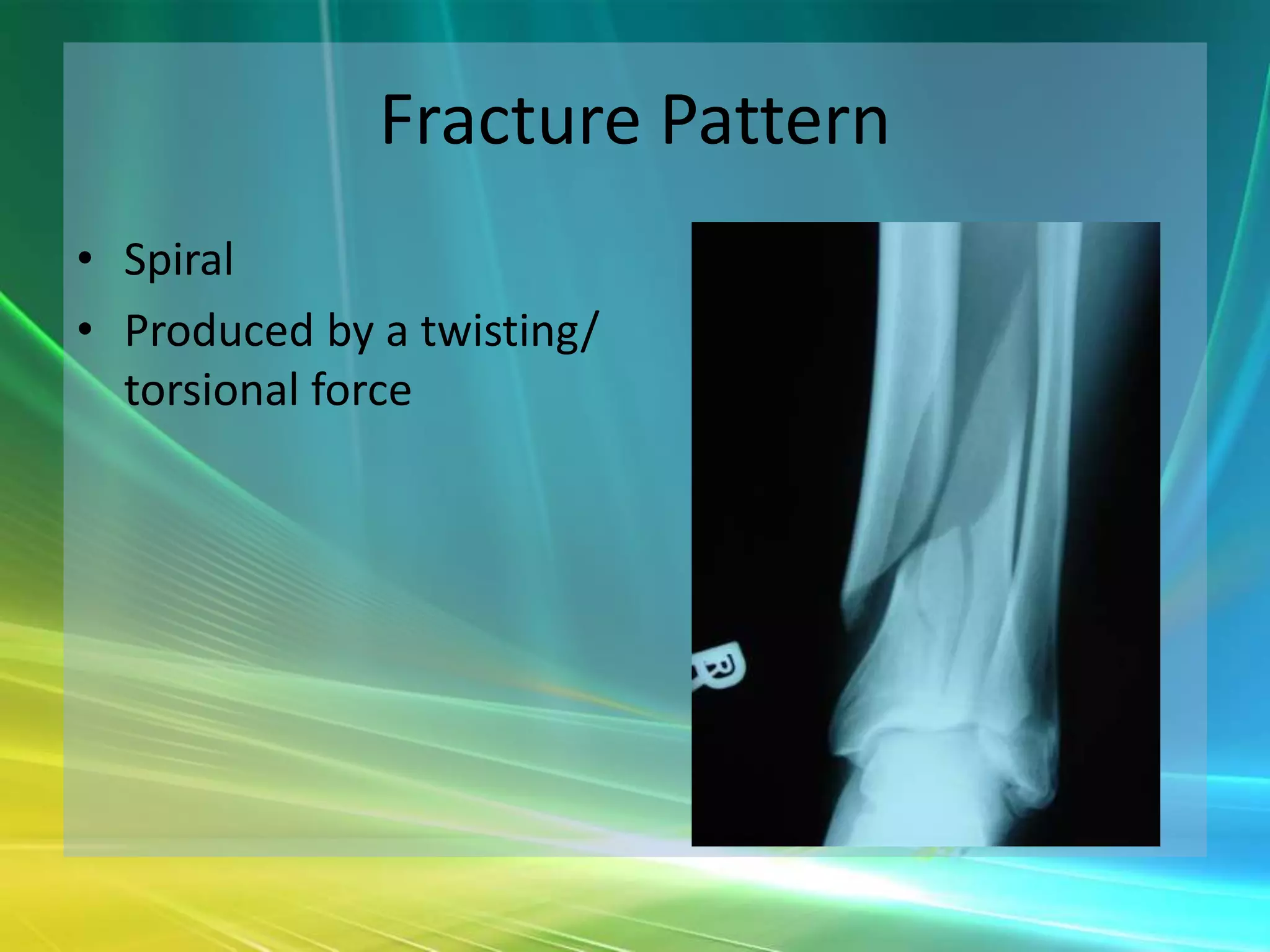
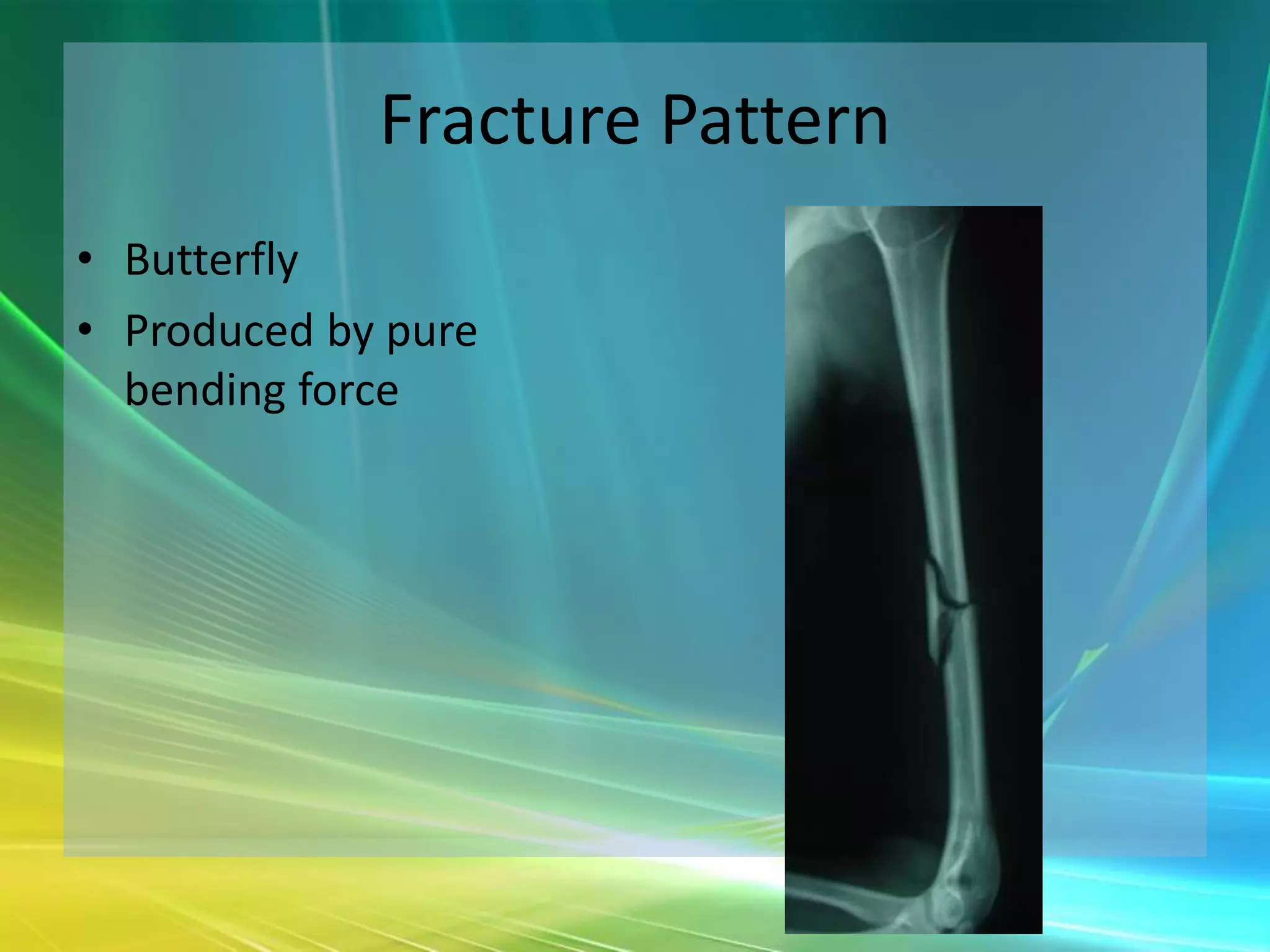
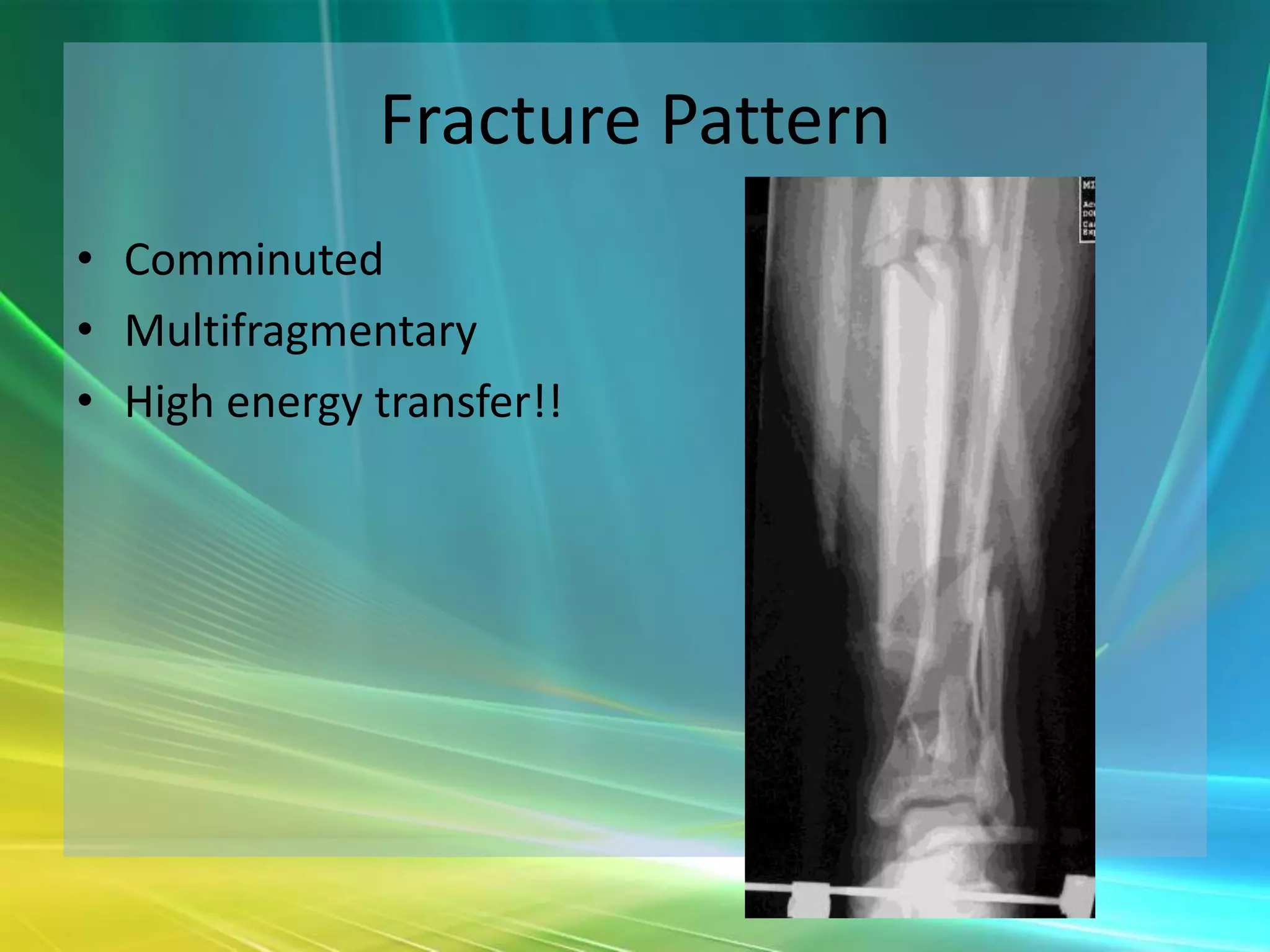
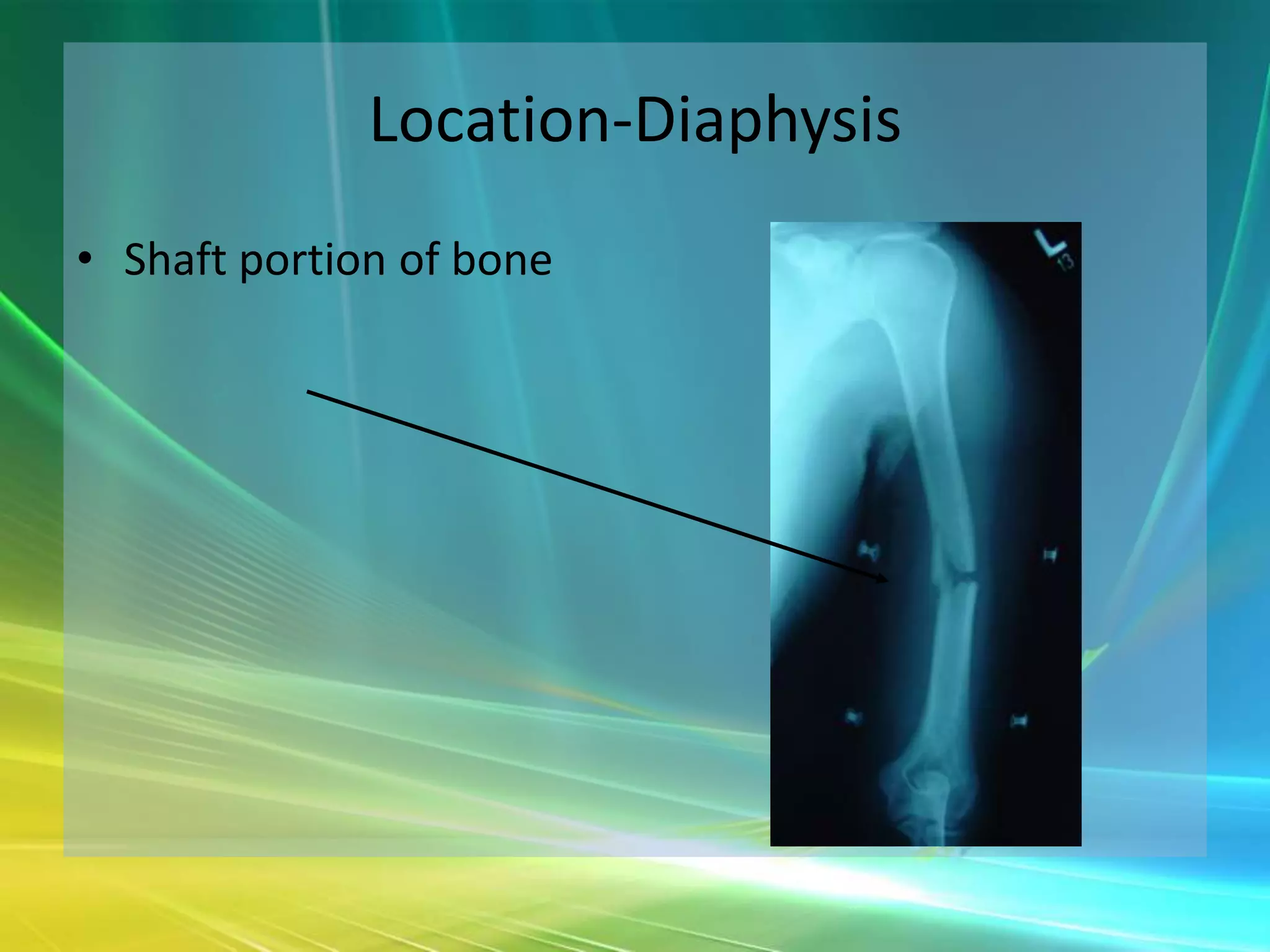
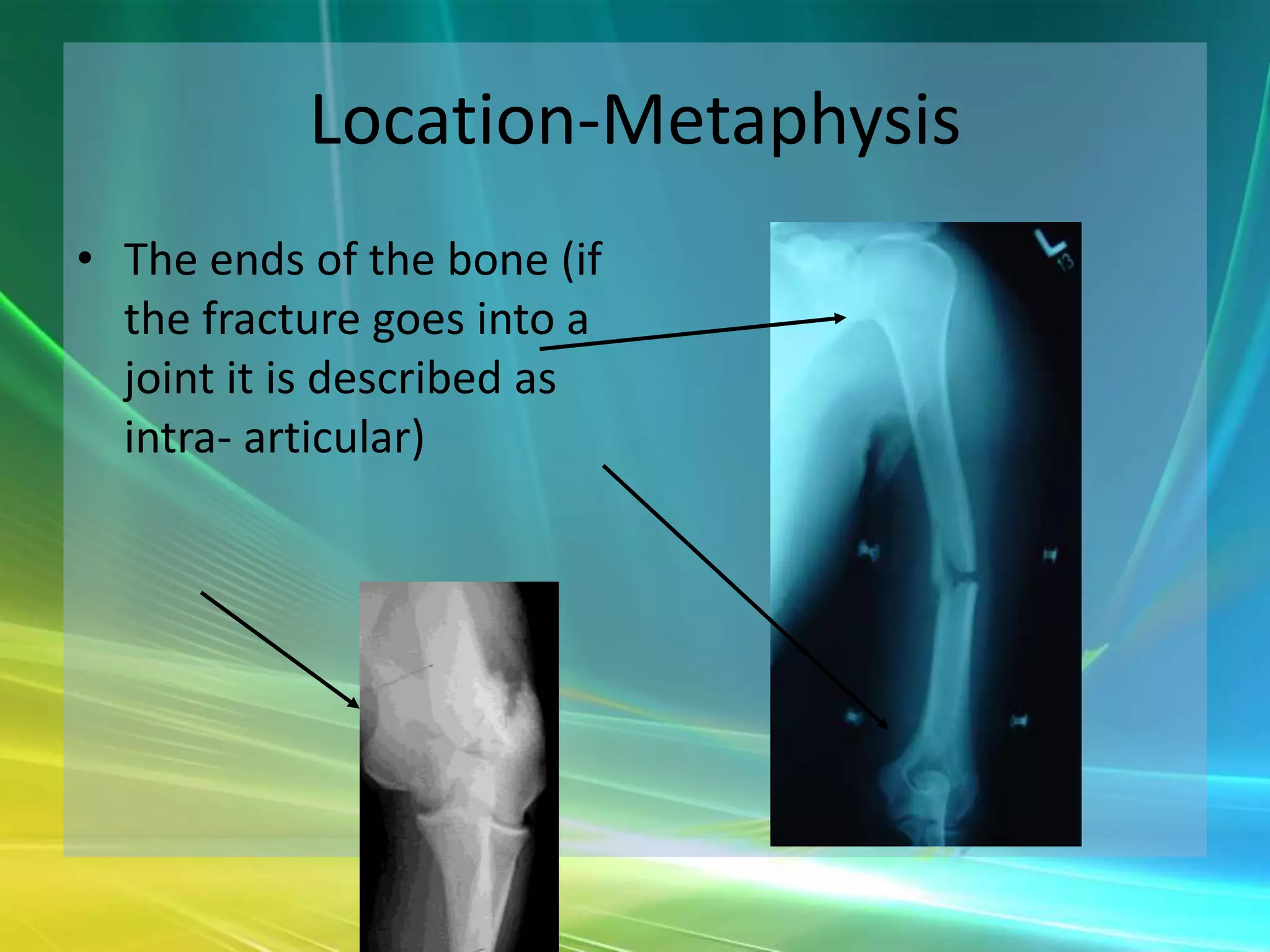
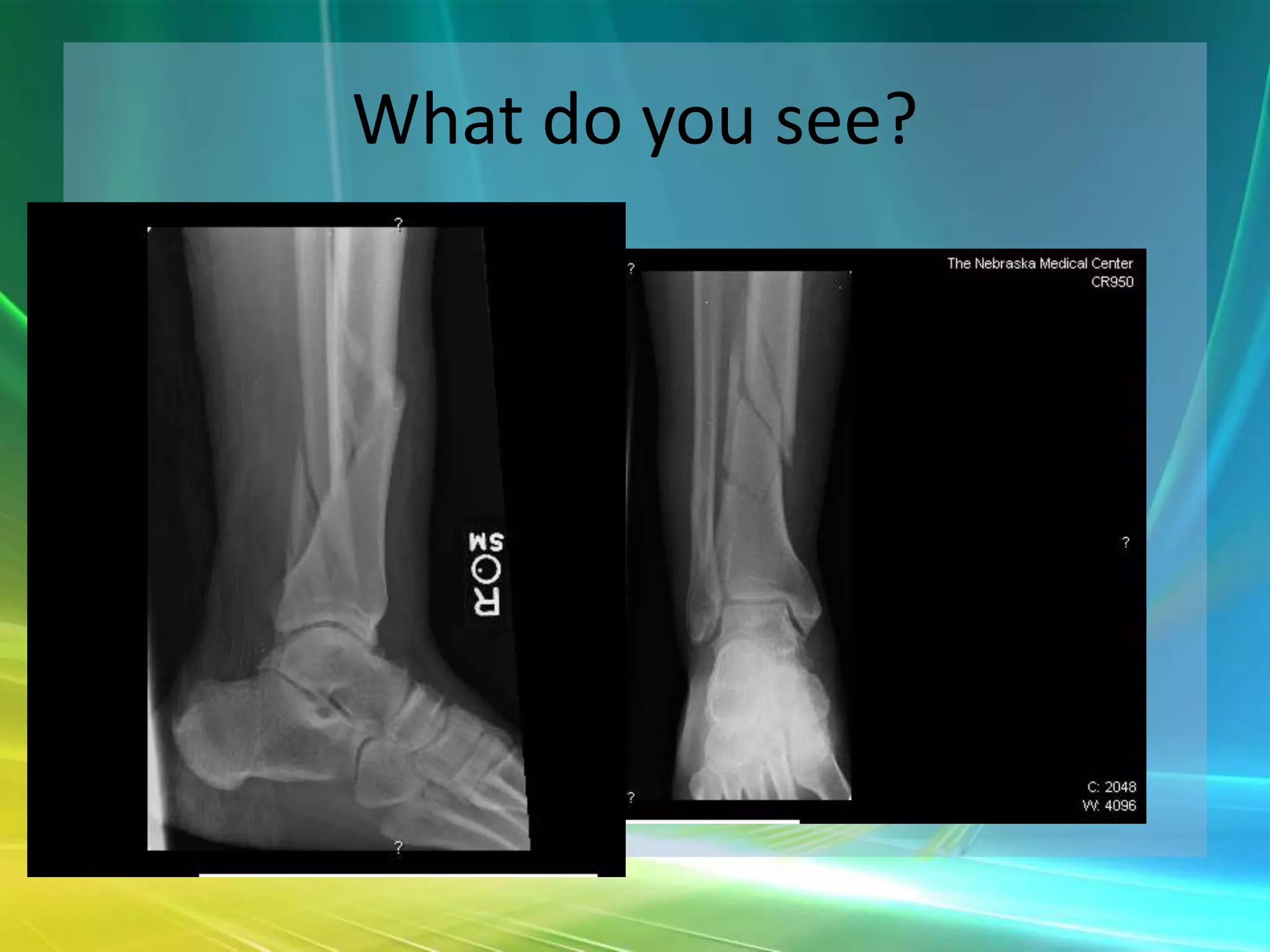
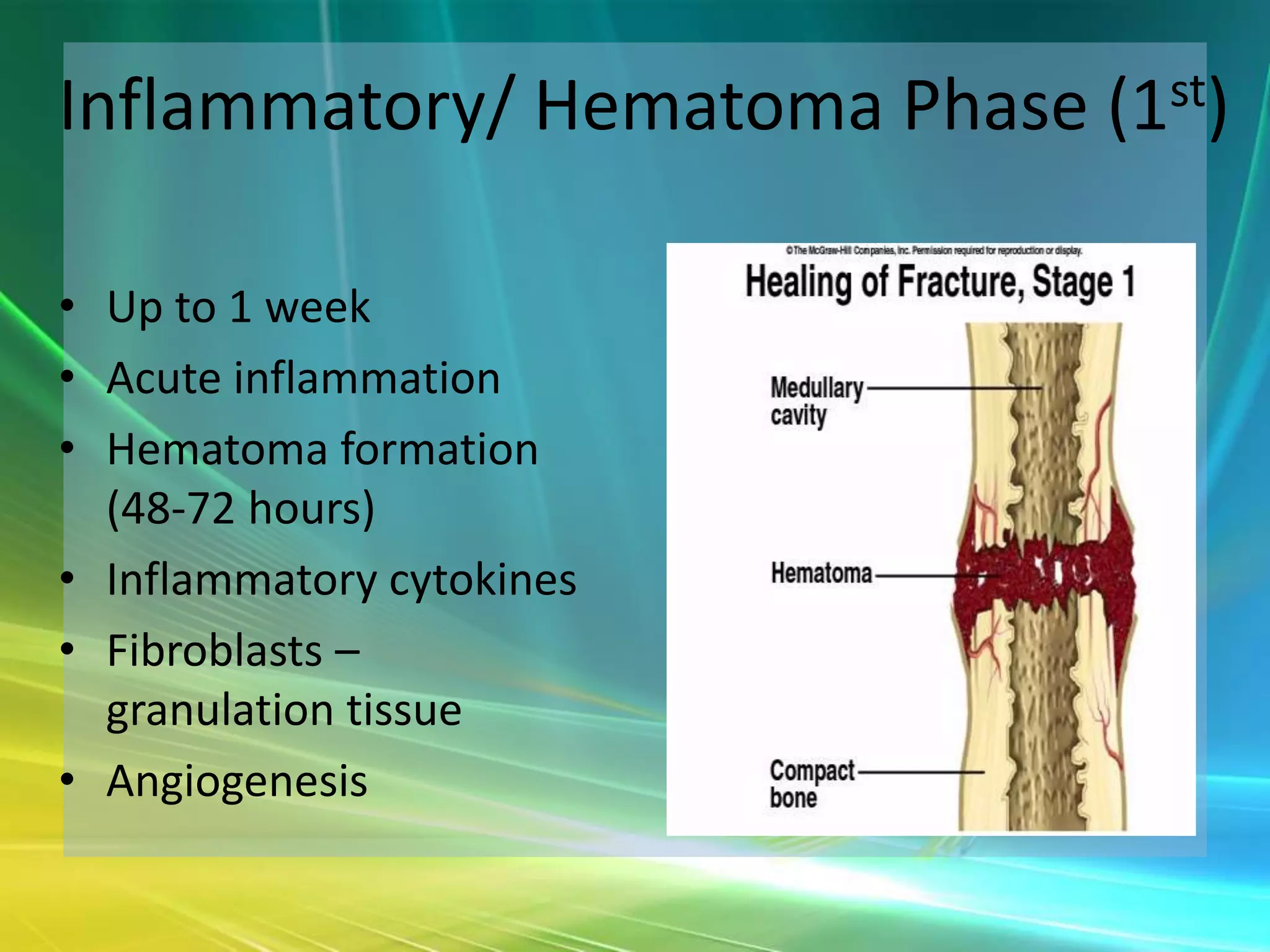
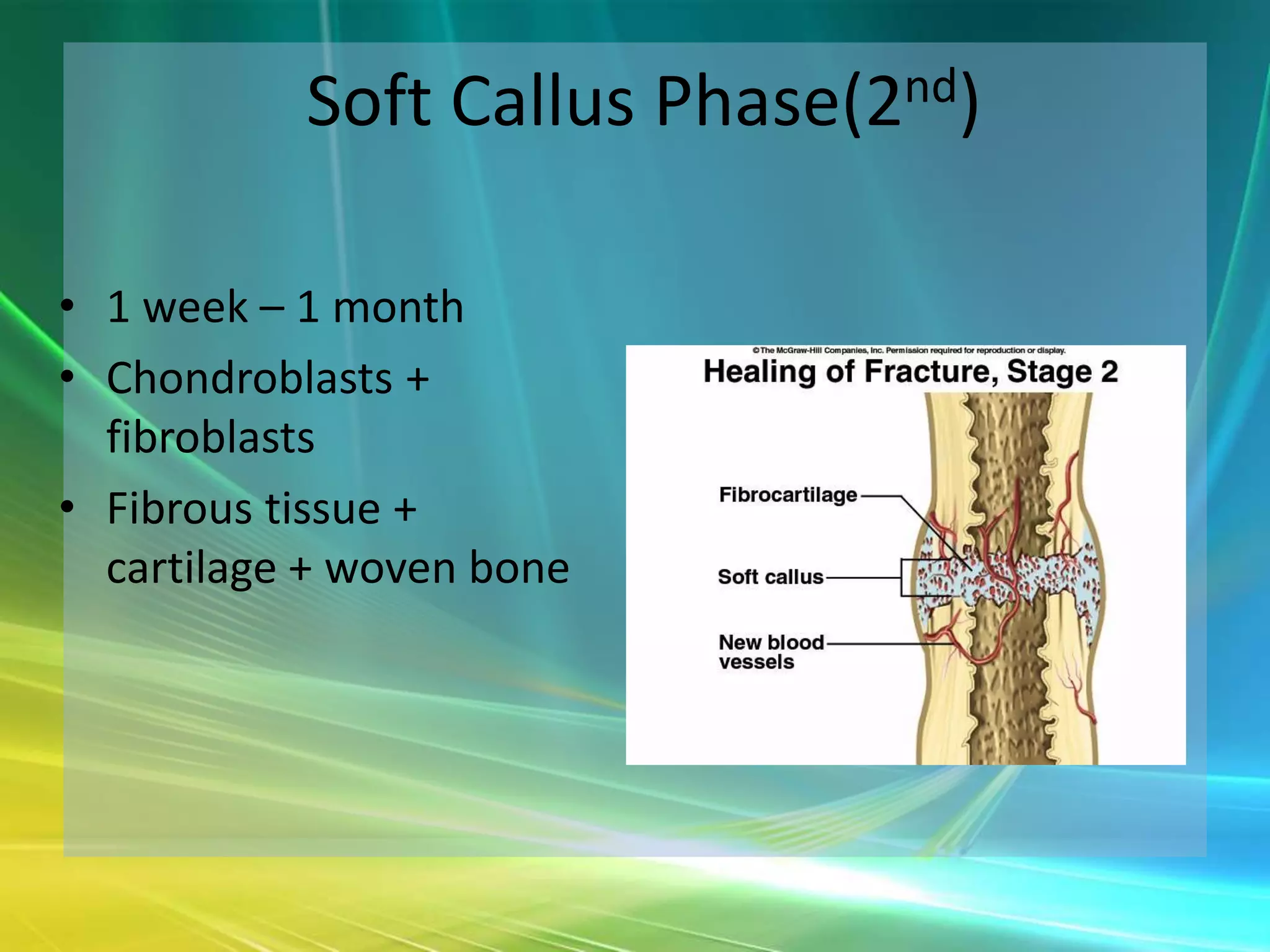
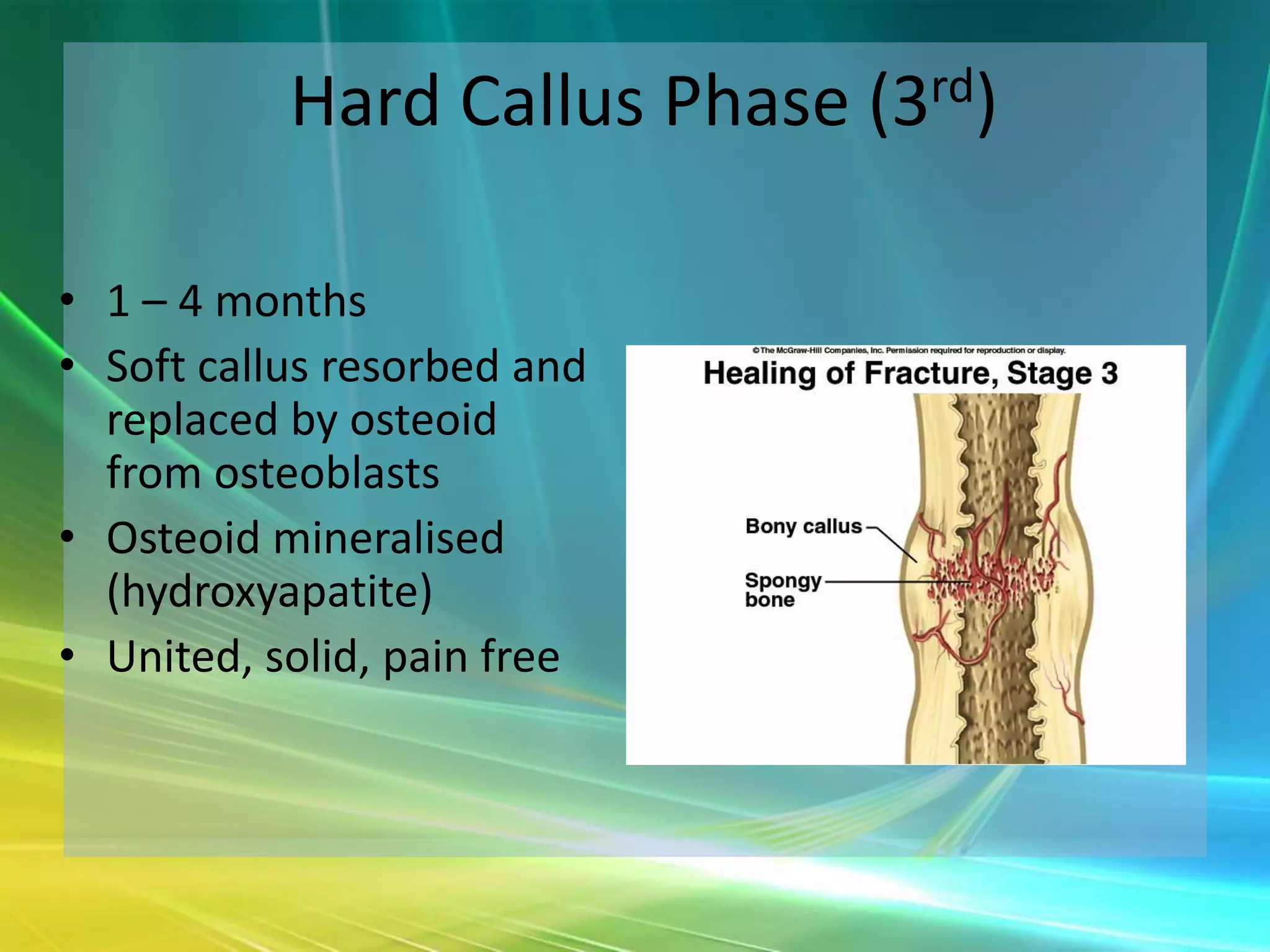
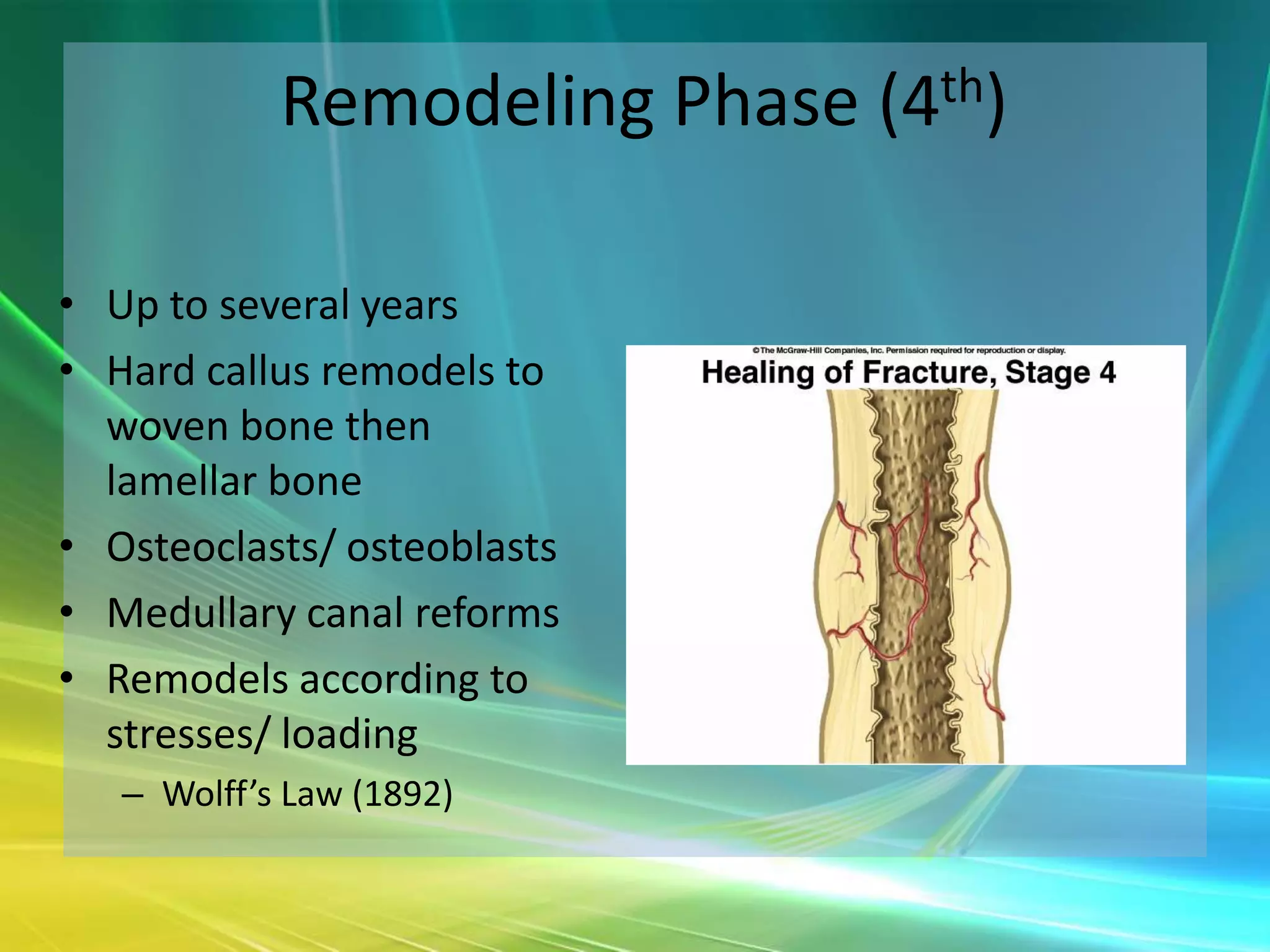
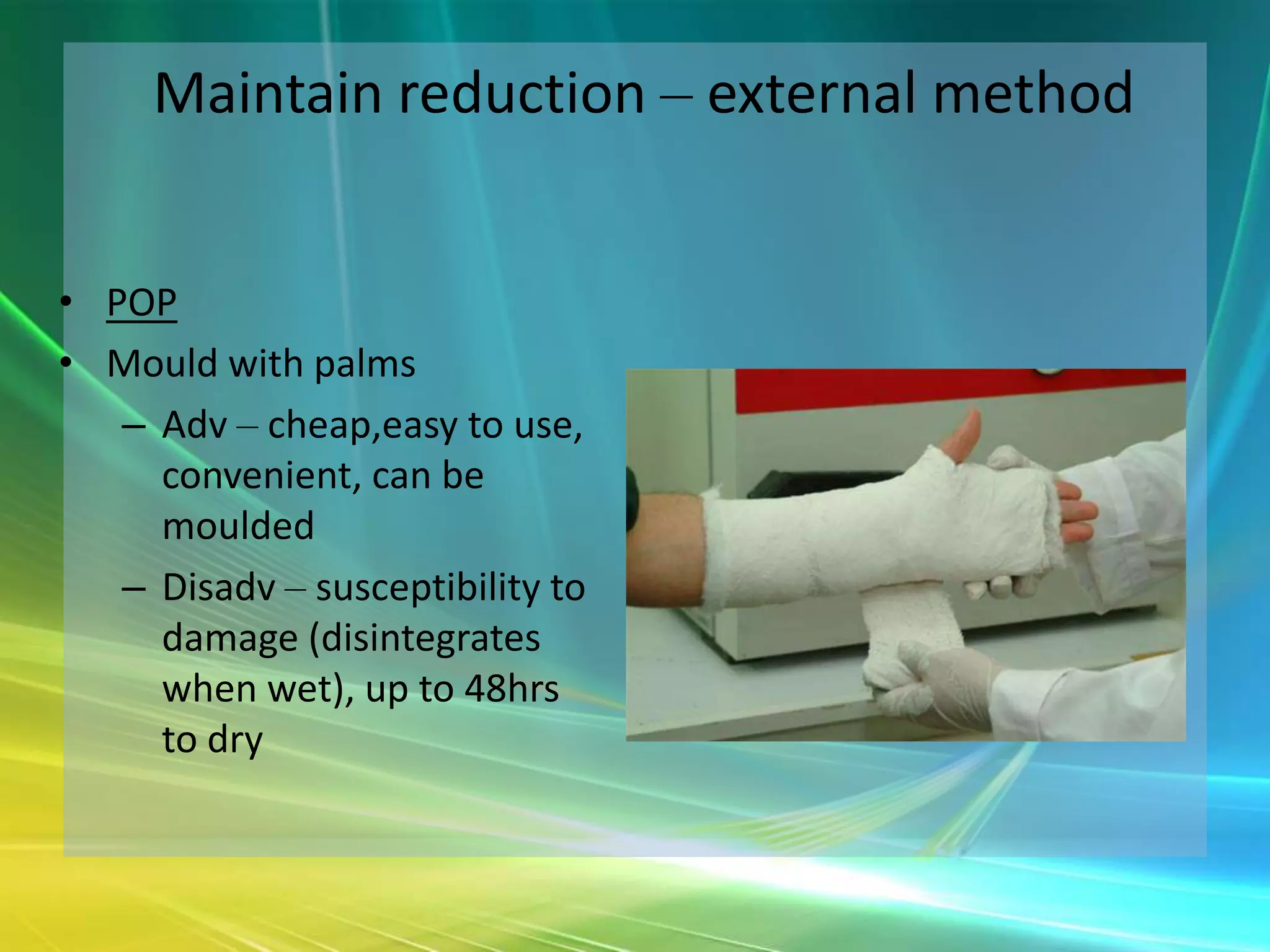
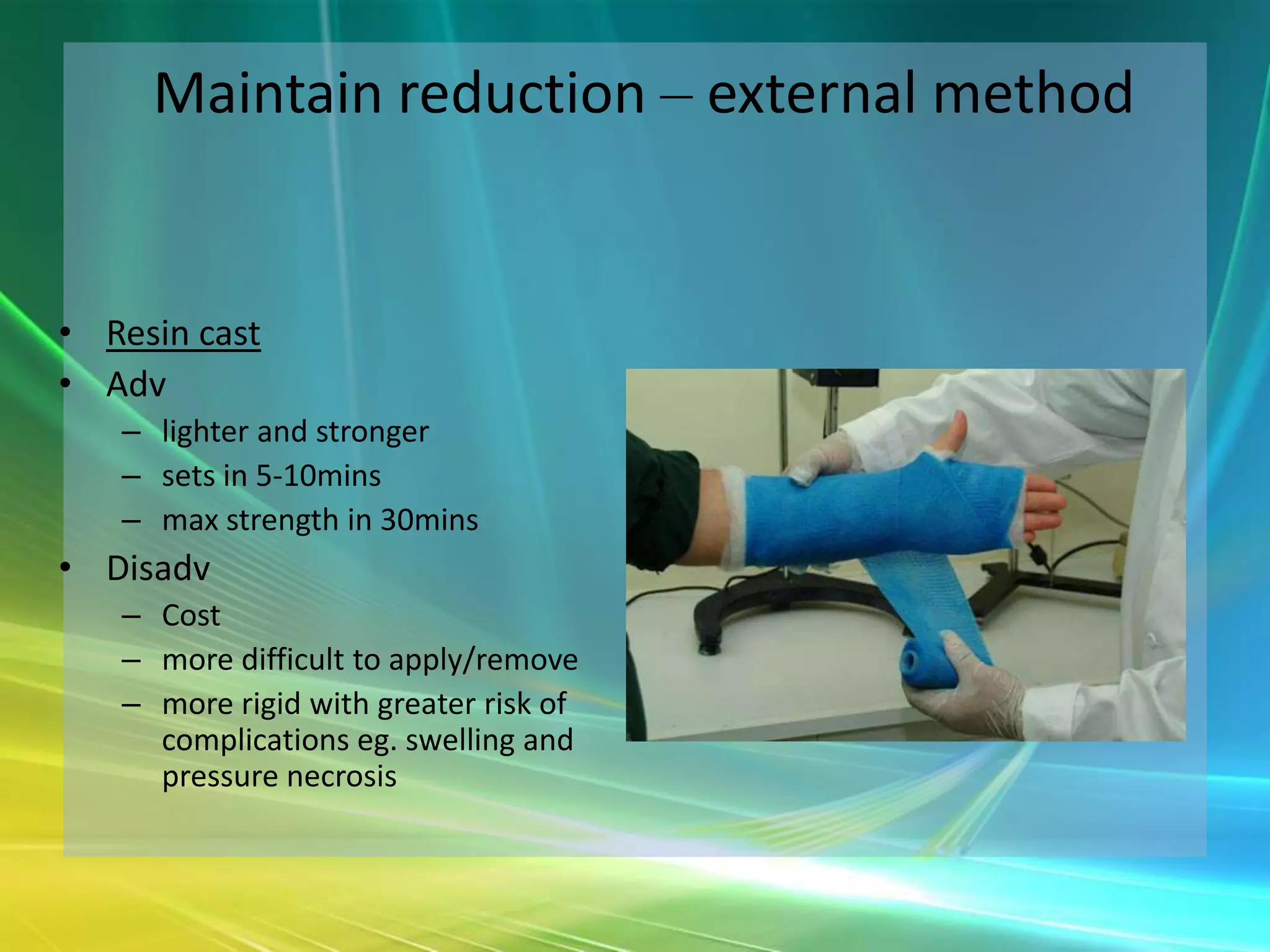
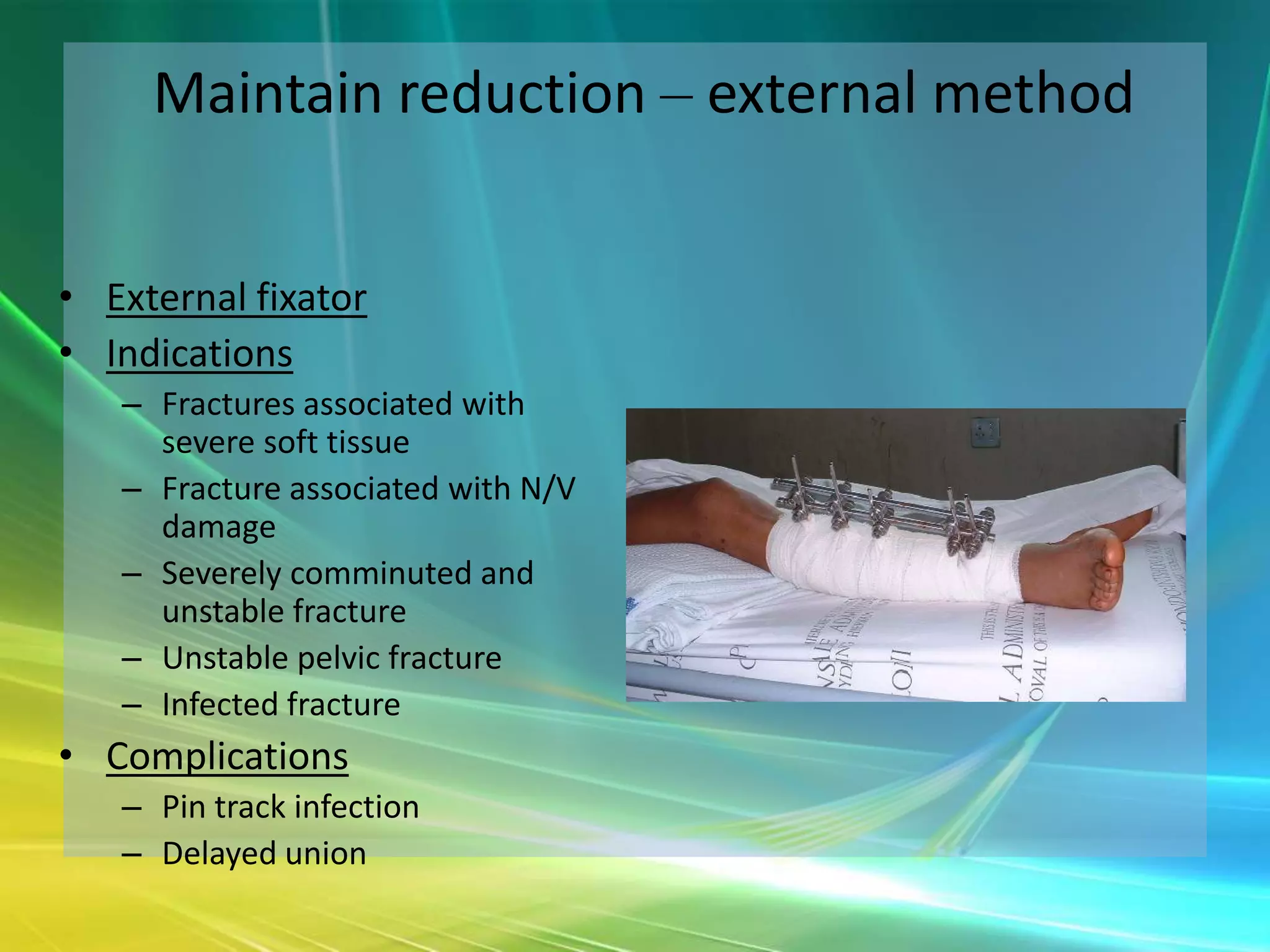
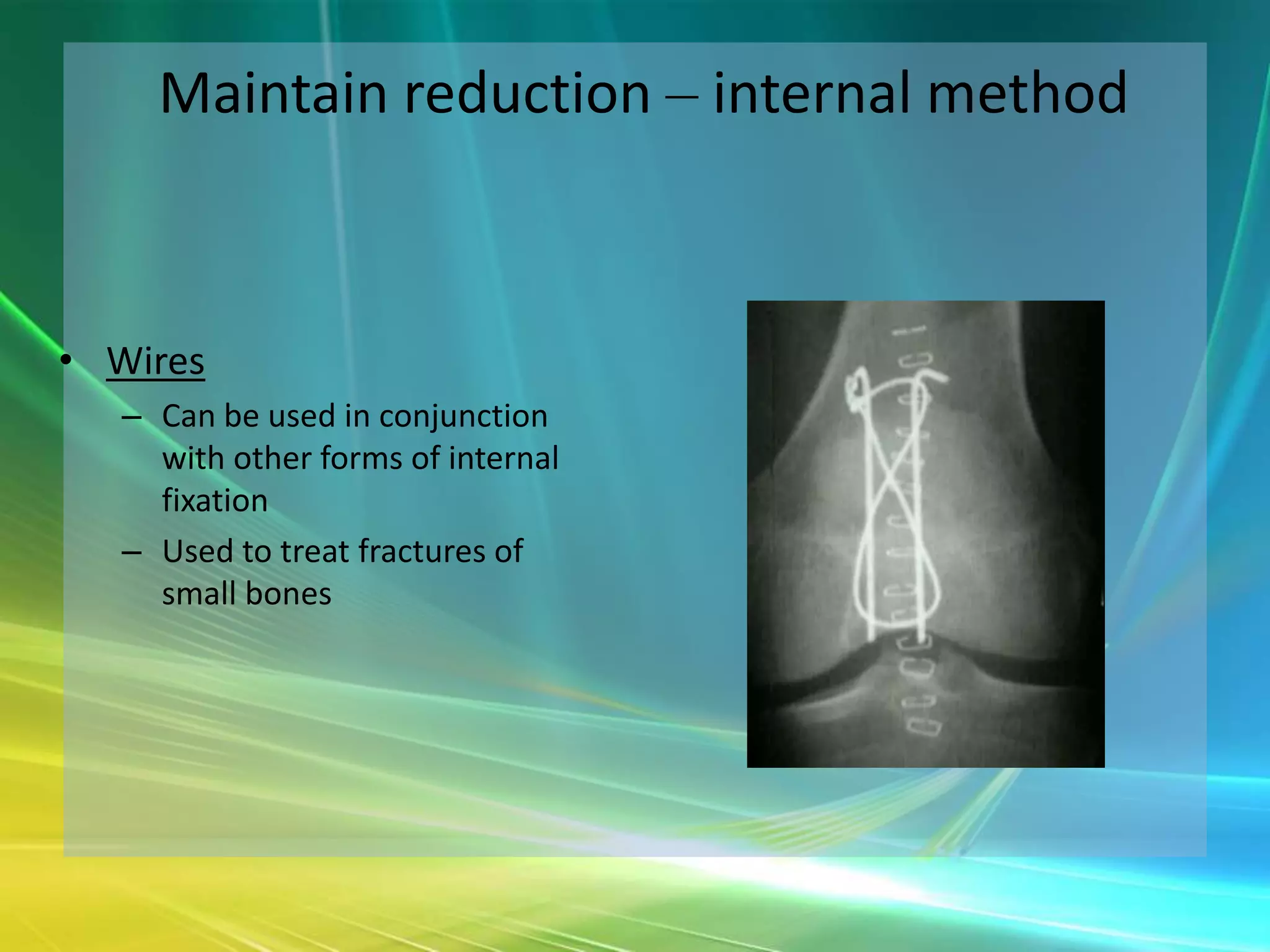
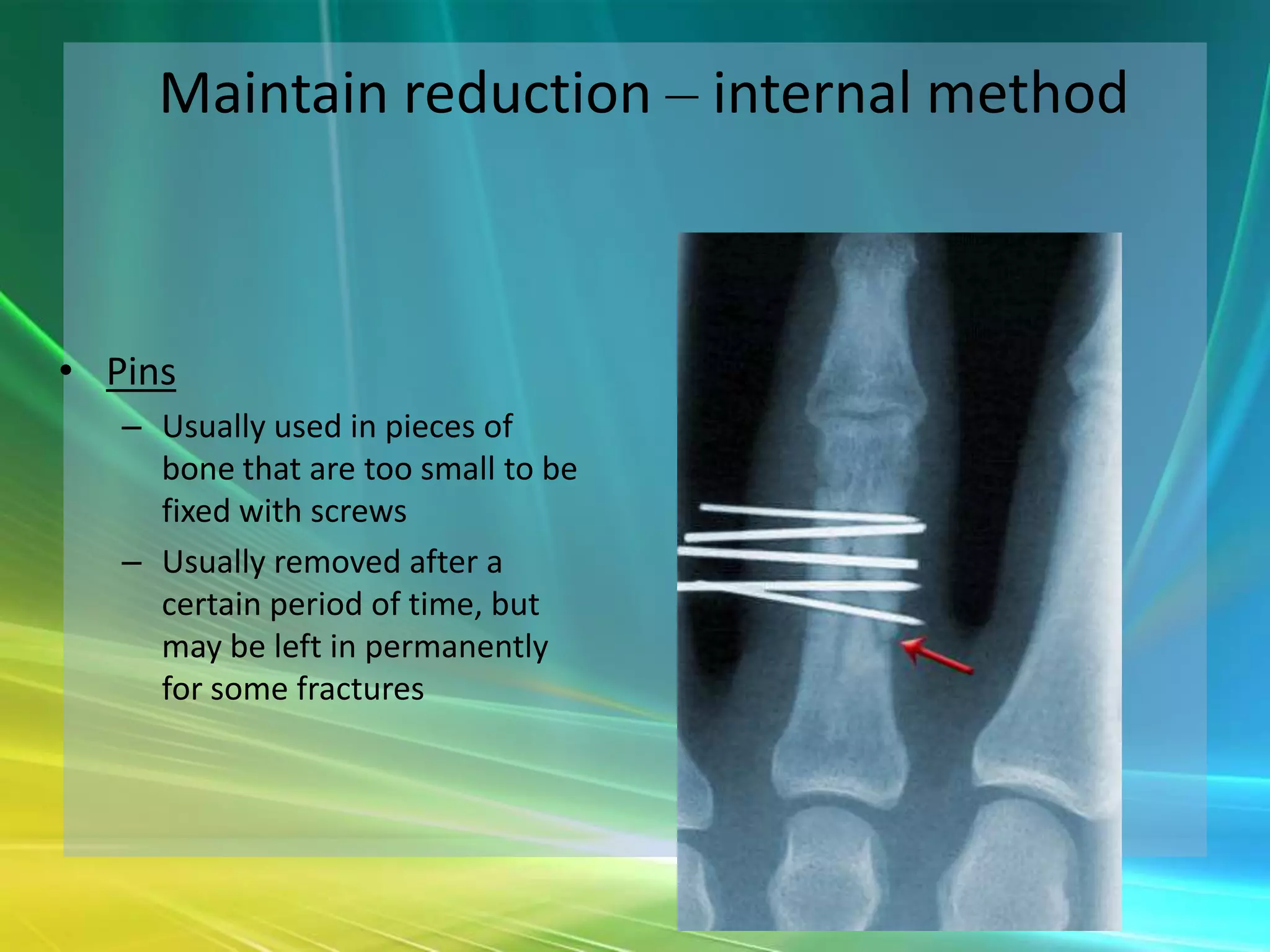
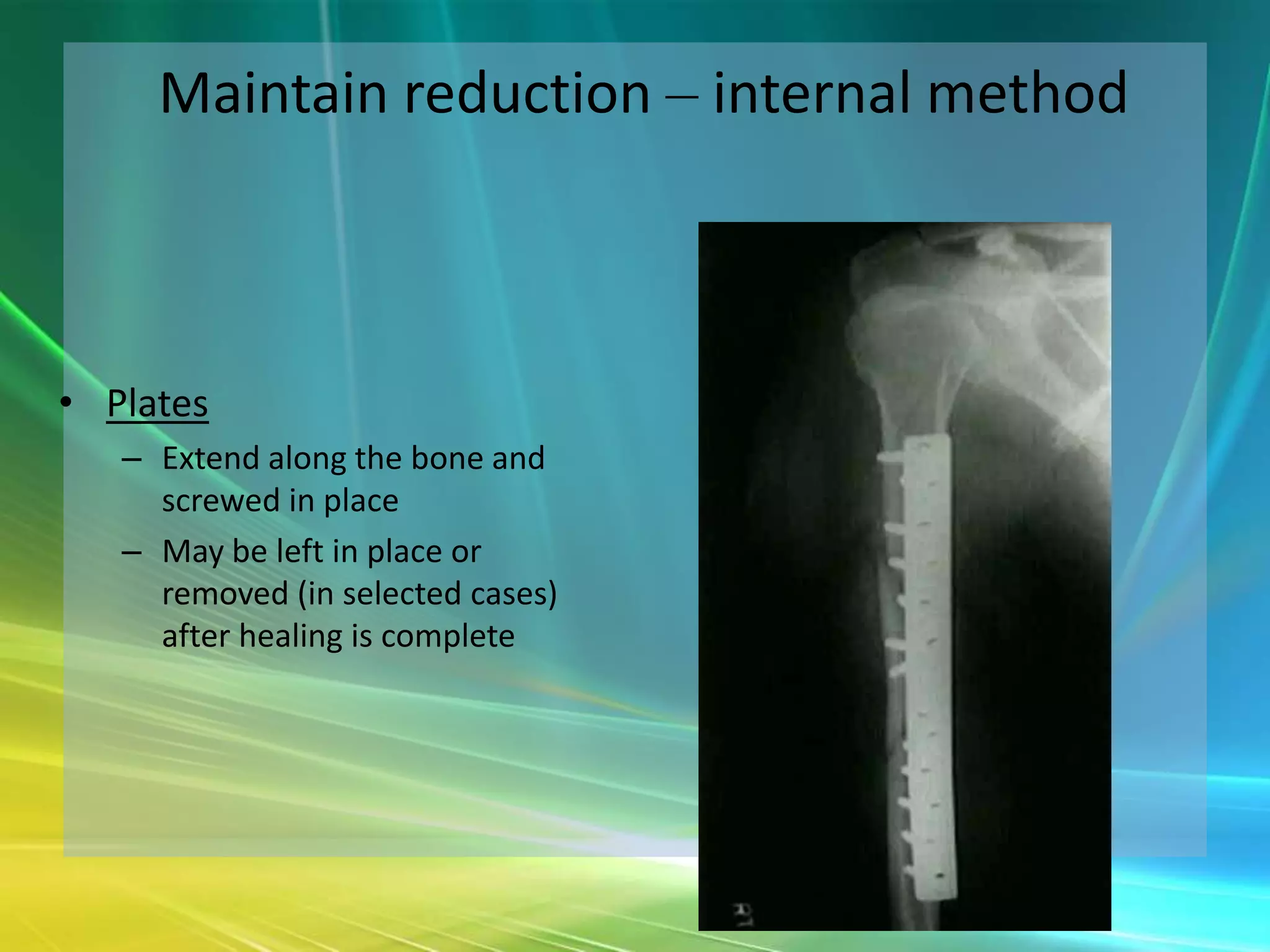
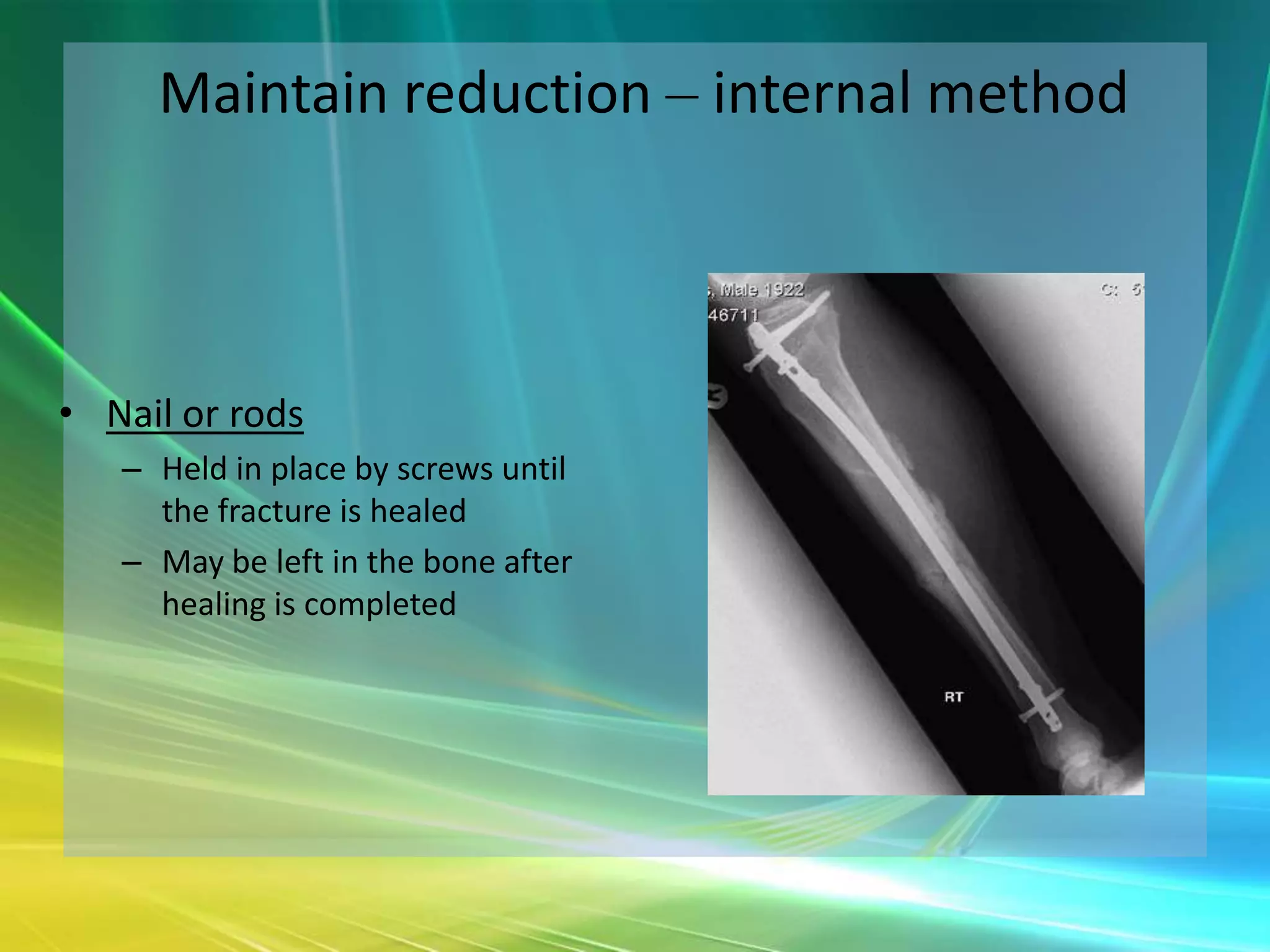
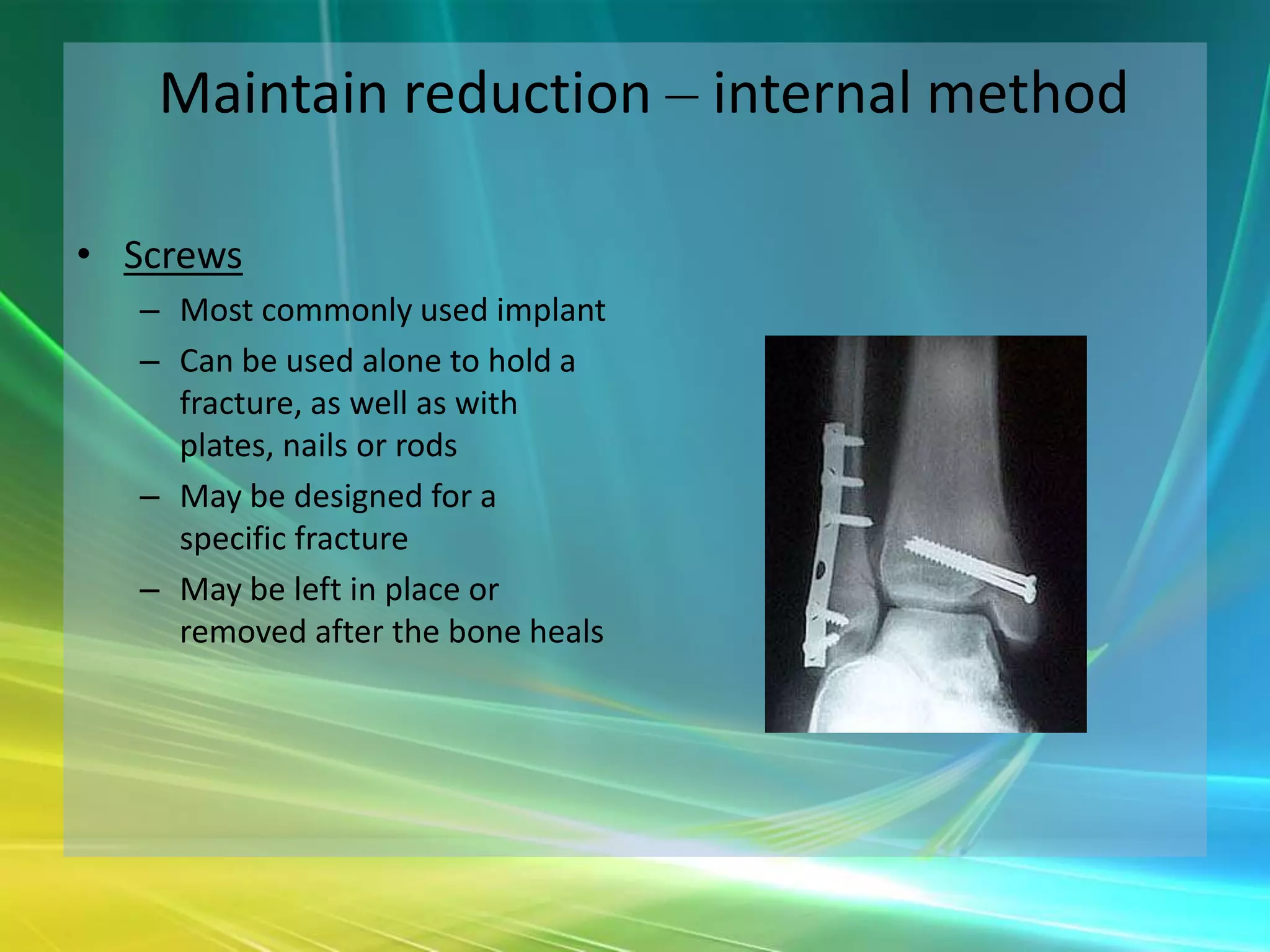
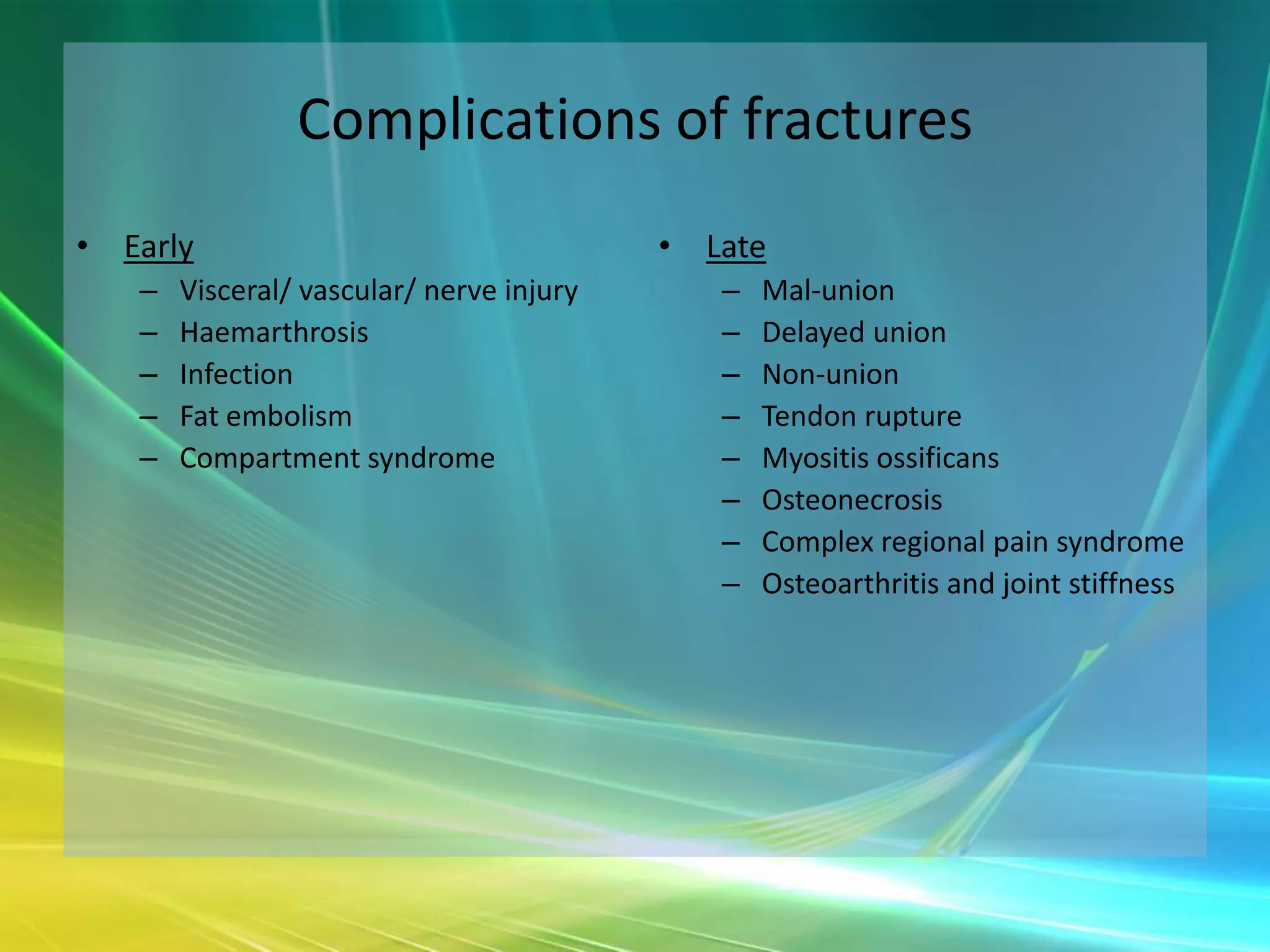
This document provides an overview of orthopaedic trauma and fracture management. It defines the golden hour of trauma and describes the ATLS protocol. It discusses the primary and secondary surveys for trauma patients. Key aspects of fracture assessment and basic fracture mechanics are reviewed. The stages of fracture healing and factors affecting healing are outlined. Methods for maintaining fracture reduction both externally (casts, traction, external fixators) and internally (wires, pins, plates, nails, screws) are summarized.