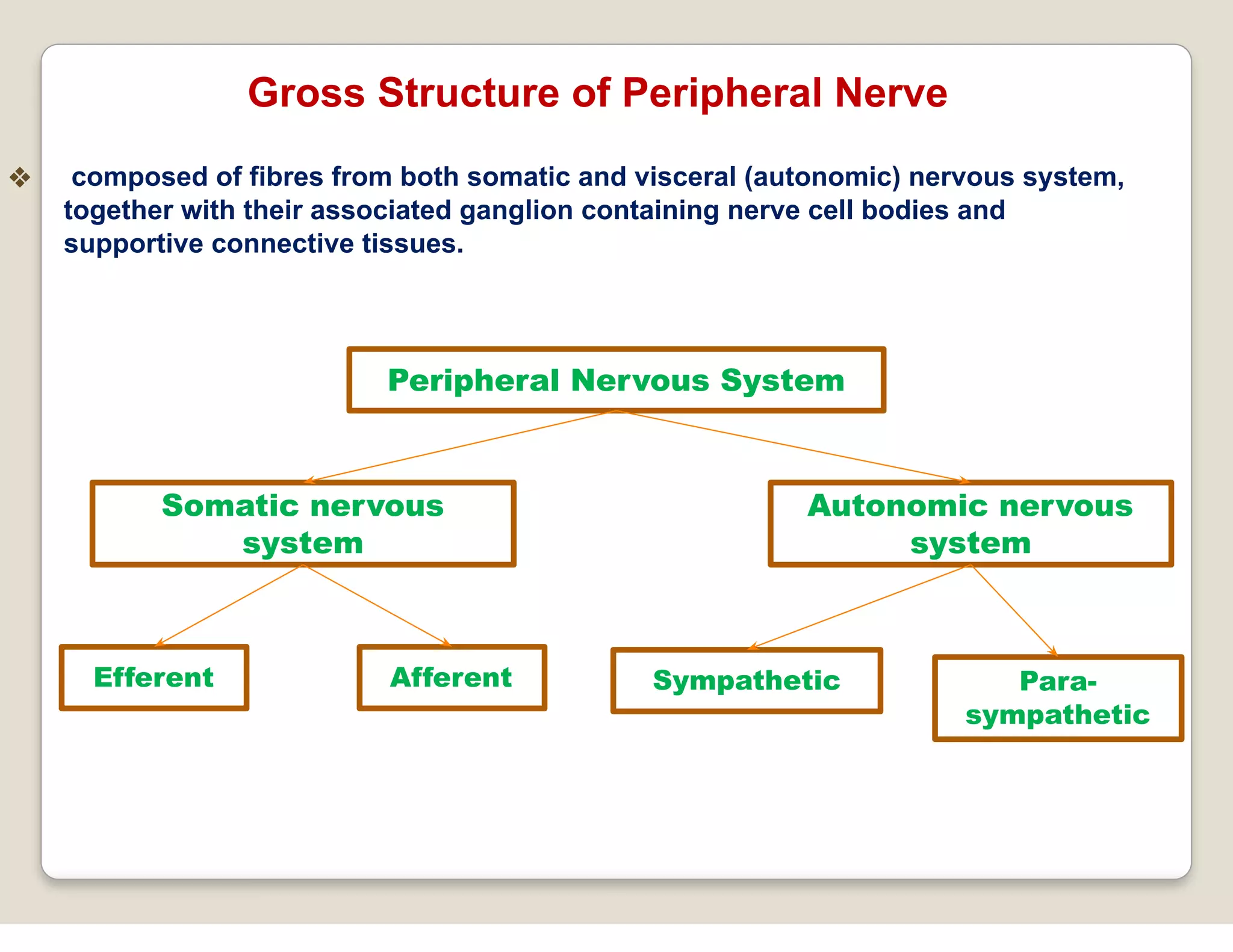
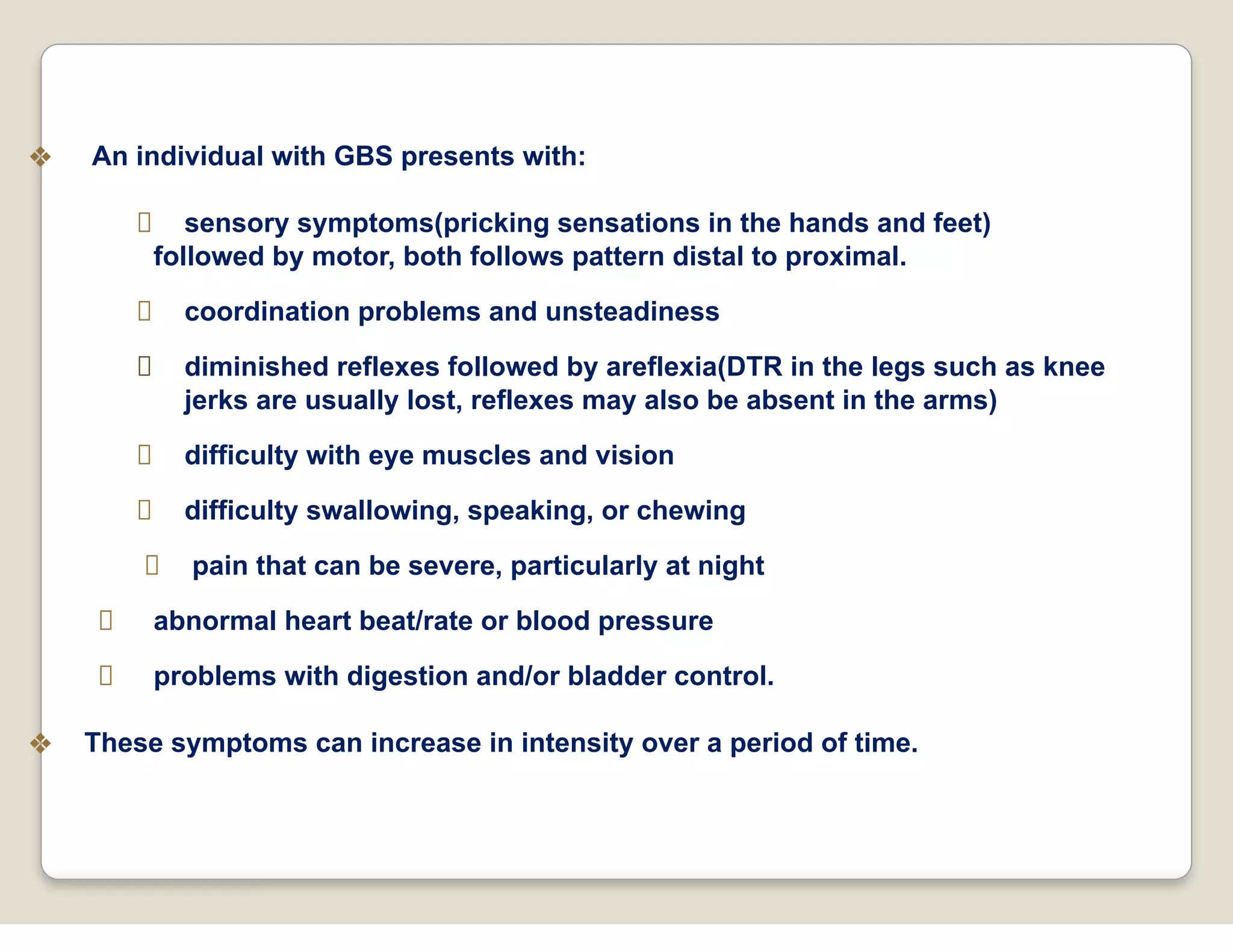
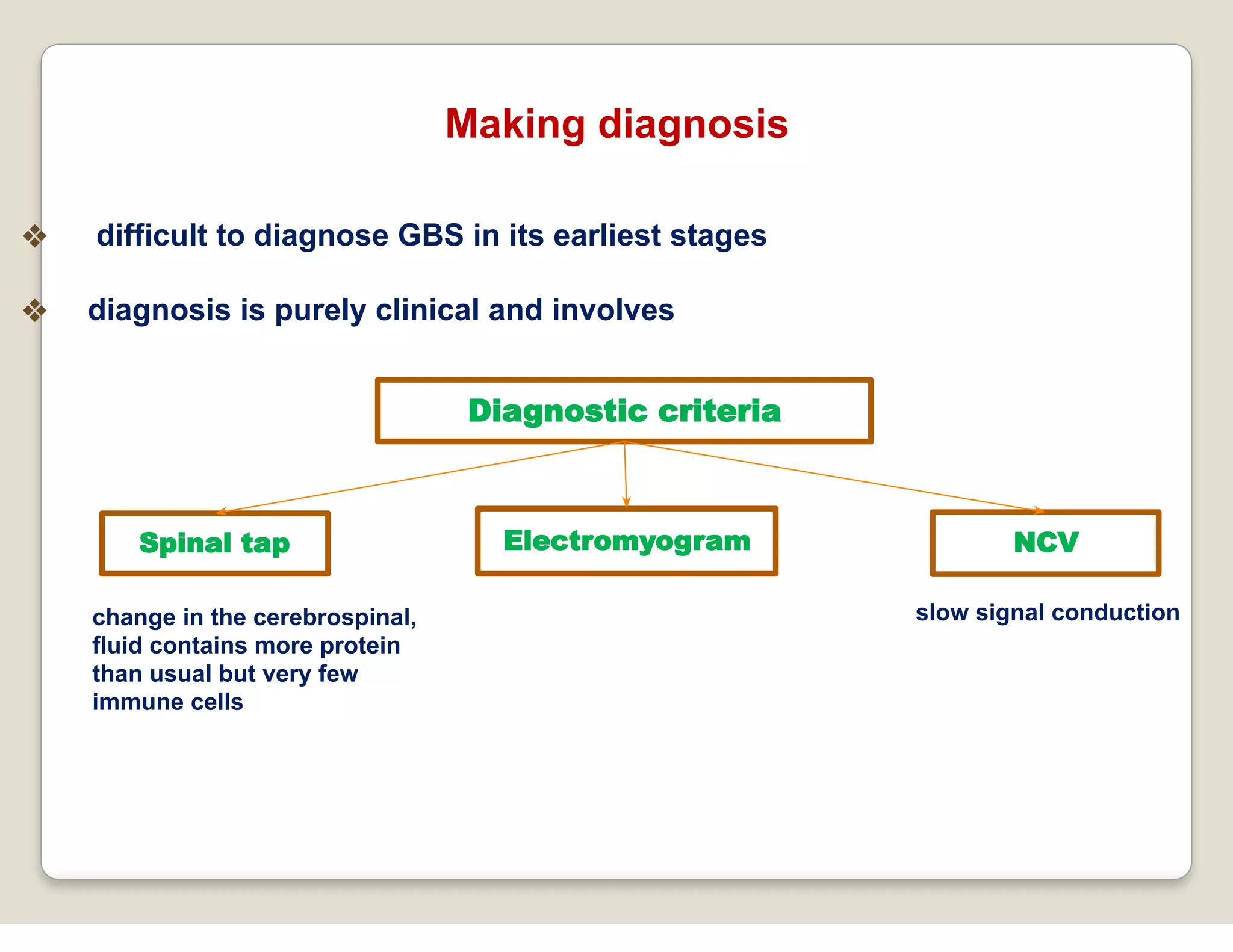
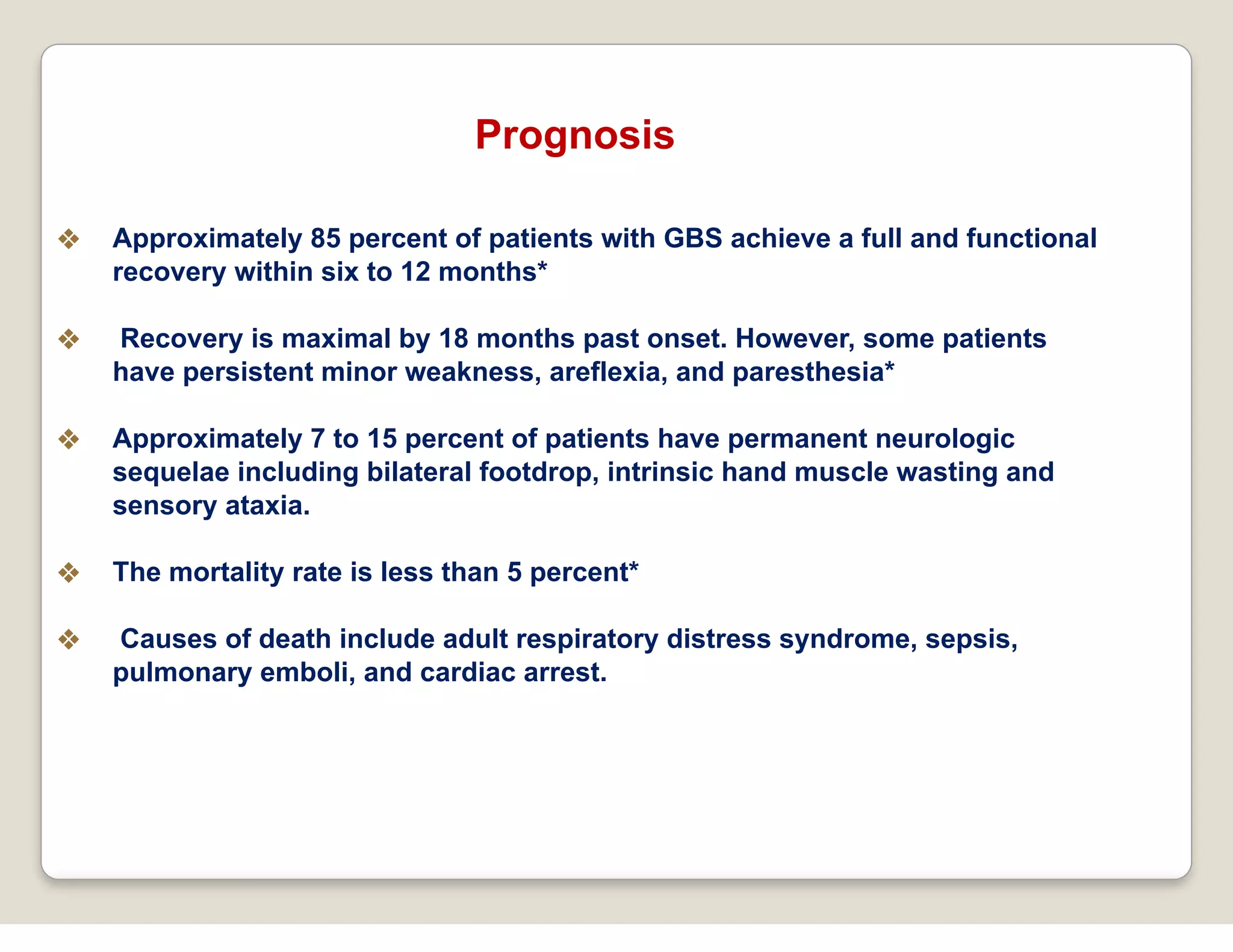
The document provides an overview of Guillain-Barré Syndrome (GBS), detailing its classification, clinical presentation, epidemiology, etiology, pathophysiology, diagnosis, treatment, and prognosis. GBS is recognized as an autoimmune disorder primarily affecting peripheral nerves, characterized by acute weakness and sensory disturbances, often following infections. Approximately 70% of affected individuals experience full recovery, though some may face long-term complications, and the document discusses modern research approaches to understanding and treating this condition.