Encephalitis is an inflammation of the brain that can be caused by viral infections or autoimmune responses. It occurs most commonly in children, the elderly, and immunocompromised individuals. Symptoms vary depending on age but may include fever, headache, confusion, seizures, and long-term neurological complications. Diagnosis involves imaging, spinal fluid analysis, and blood tests to identify potential causes. Treatment focuses on supportive care and antiviral medications or antibiotics depending on the suspected cause. Outcomes range from full recovery to permanent neurological deficits and risk of death is highest in cases of prolonged coma or infection with herpes simplex virus.
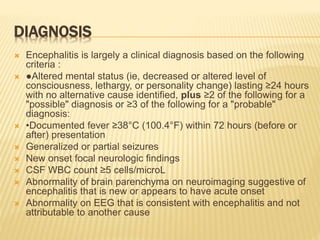
![TYPE OF AUTOIMMUNE ENCEPHALITIS
Acute Disseminated Encephalomyelitis (ADEM)
NMDA Receptor associated Encephalitis [N-
methylD-aspartate (NMDA) ]
EEG “extreme delta brush”, Brain MRI: non specific ,CSF: pleocytosis and/or
protein in>80%, NMDAR antibodies in CSF or serum.
Hashimoto’s Encephalopathy
Hypothyroidism 50% ,MRI often normal,EEG: slow activity ,CSF:elevated protein
Rasmussen Encephalitis
Progressive refractory partial seizures, cognitive decline, focal deficits, and
brain hemi atrophy
MRI: progressive unilateral hemispheric atrophy
LIMBIC ENCEPHALITIS
Hyponatremia, dystonic or myoclonic-like movements, described as
faciobrachial dystonic seizures,with EEG features of tonic seizures.](https://image.slidesharecdn.com/encephalitis-190519080519/85/Encephalitis-9-320.jpg)

![NEONATES AND YOUNG INFANTS
the presentation of encephalitis can be nonspecific.
Encephalitis should be considered in a neonate or
young infant who has
fever, seizure, poor feeding, irritability, or lethargy, a
full or bulging fontanel Decreased perfusion may
occur in infants with encephalitis and viral infection
(eg, herpes simplex virus [HSV]), crying that doesn't
stop or that seems worse when an infant is picked
upor handled in some way .
Fever is a variable finding. Neonates who have viral
illness, especially HSV and enterovirus, are at risk for
severe central nervous system and systemic illness](https://image.slidesharecdn.com/encephalitis-190519080519/85/Encephalitis-12-320.jpg)