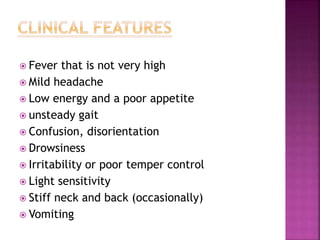
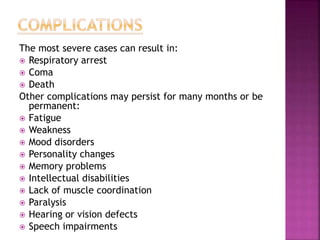
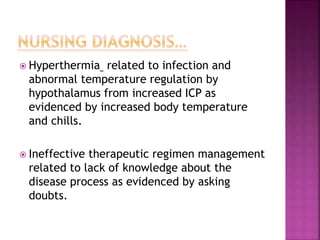
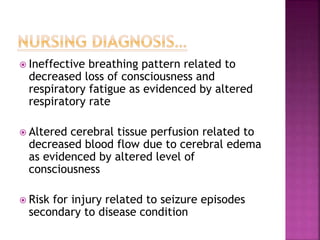
The document discusses meningitis and encephalitis. It defines meningitis as an inflammation of the protective membranes covering the brain and spinal cord, known as the meninges. There are various causes of meningitis including bacterial, viral, parasitic and non-infectious. Common symptoms include headache, fever and neck stiffness. Diagnosis involves spinal fluid analysis and imaging. Treatment depends on the cause but may include antibiotics, antivirals or antifungals. Encephalitis additionally involves inflammation of the brain tissue and can be caused by viruses, bacteria, parasites and fungi. It presents with fever and neurological symptoms. Treatment focuses on the underlying cause and management of symptoms.