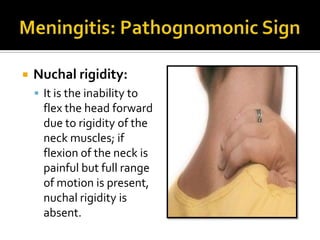
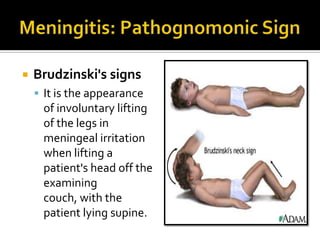
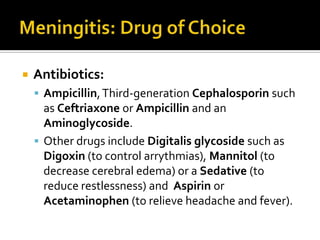
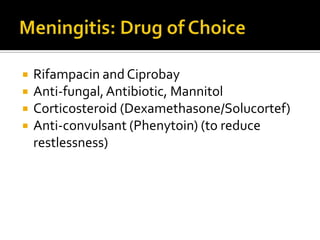
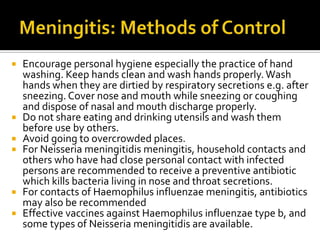
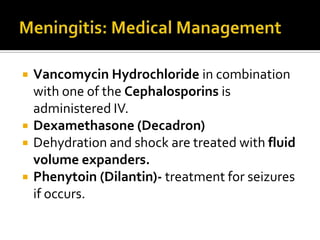
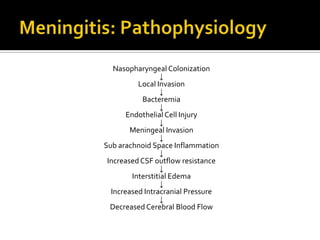
Meningitis is an infection of the meninges that covers the brain and spinal cord. It can be caused by bacteria like Neisseria meningitidis or viruses. Symptoms include headache, fever, and nuchal rigidity. Diagnosis involves lumbar puncture and imaging. Treatment involves antibiotics, steroids, and IV fluids. People remain contagious until 24-48 hours after antibiotics. Vaccines prevent certain bacterial causes.