1) Encephalitis presents as diffuse or focal neurological dysfunction that often involves the brain and meninges. Common early symptoms include fever, headache, nausea and various flu-like symptoms.
2) West Nile virus and St. Louis encephalitis virus are mosquito-borne flaviviruses that can cause encephalitis. Signs of infection include encephalopathy, neck stiffness, photophobia, seizures and paralysis.
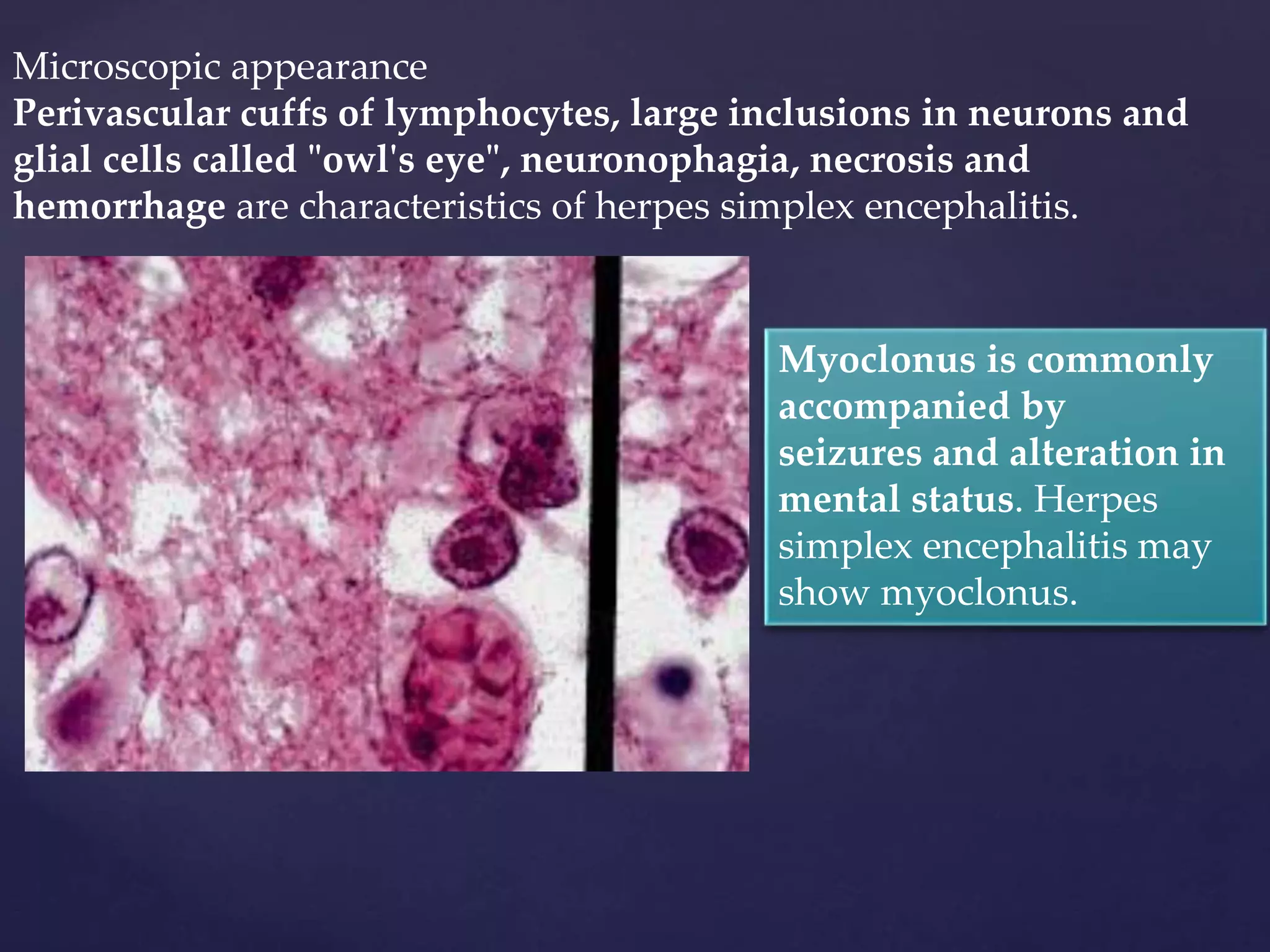
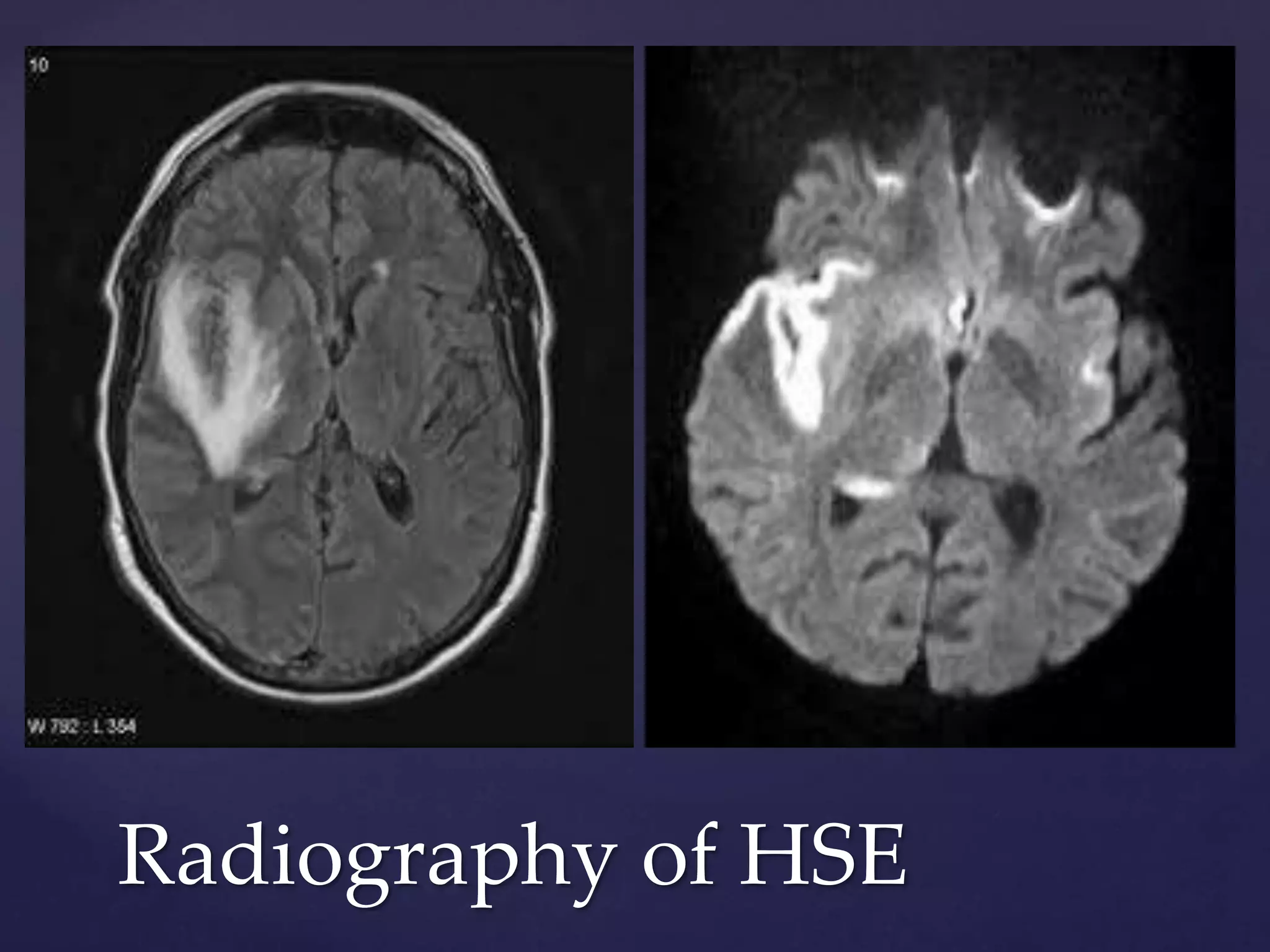
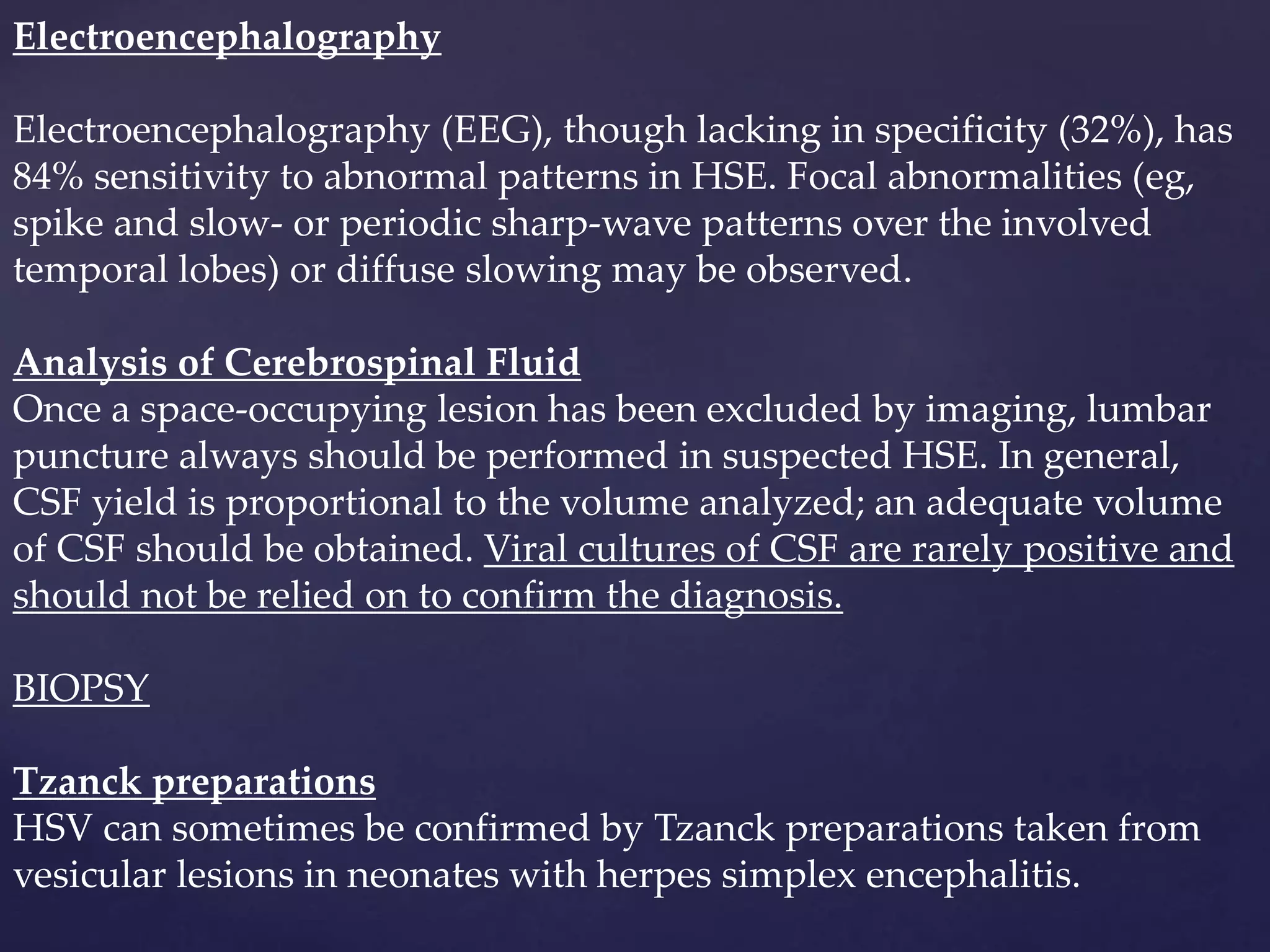
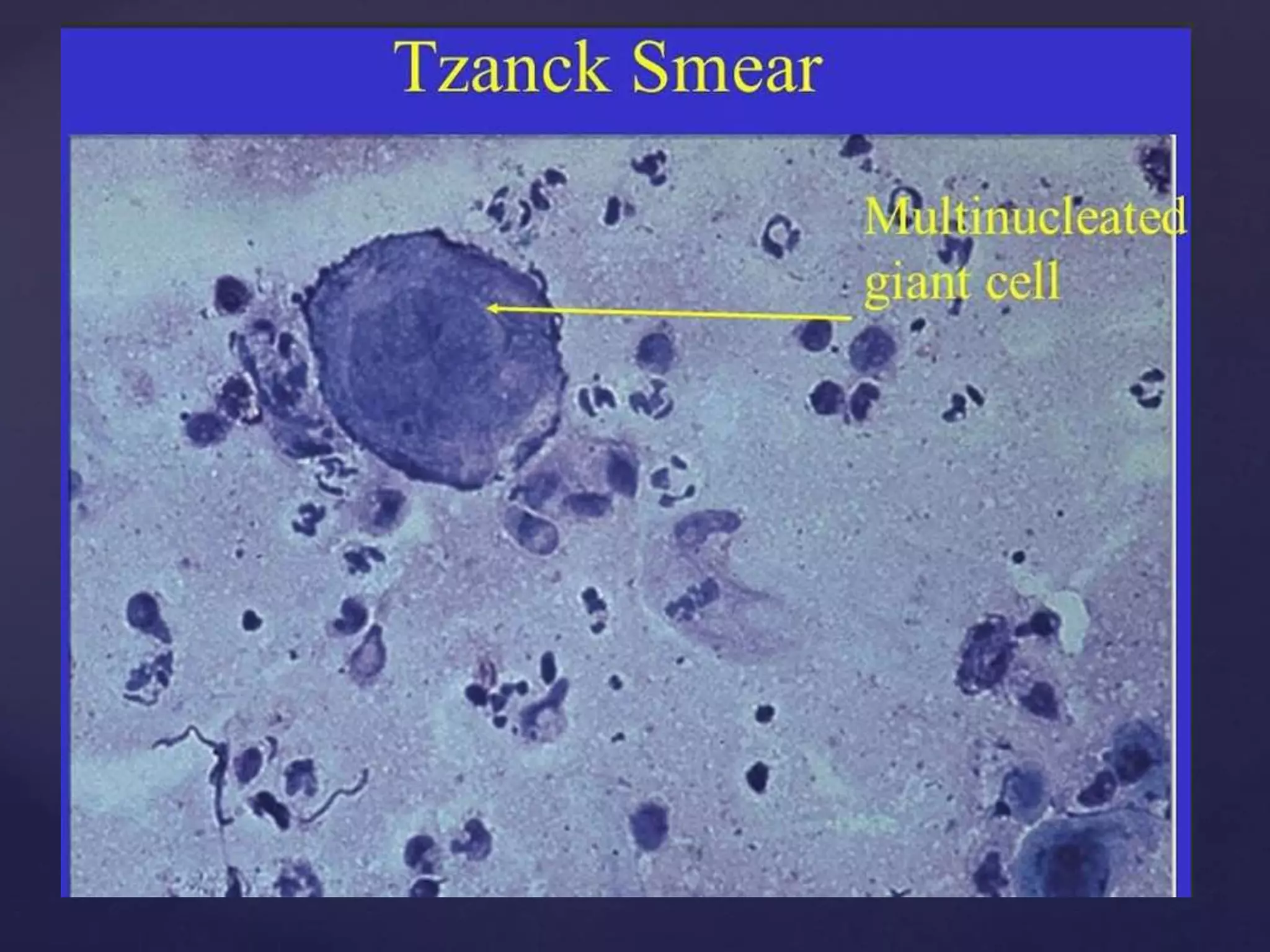
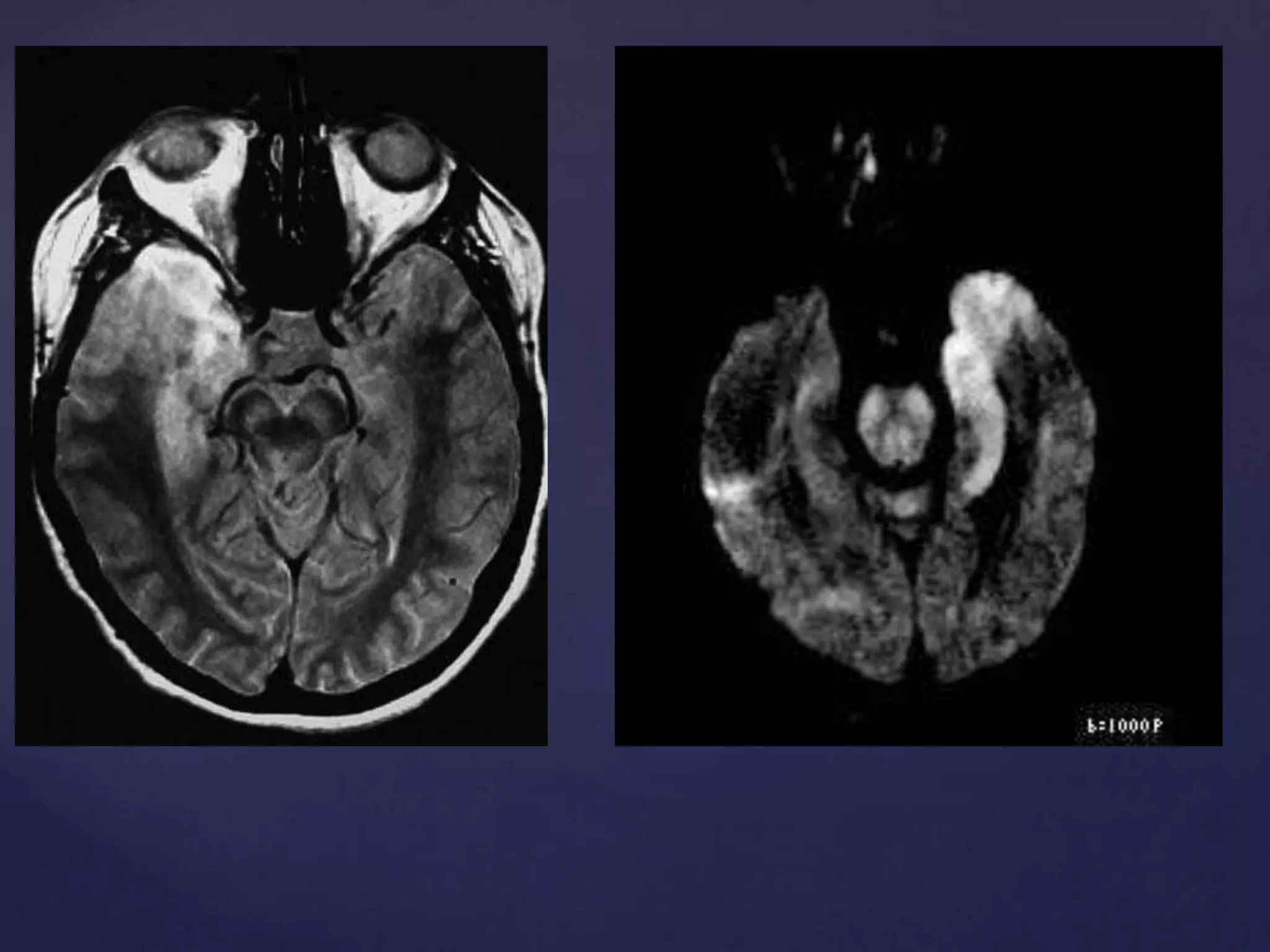
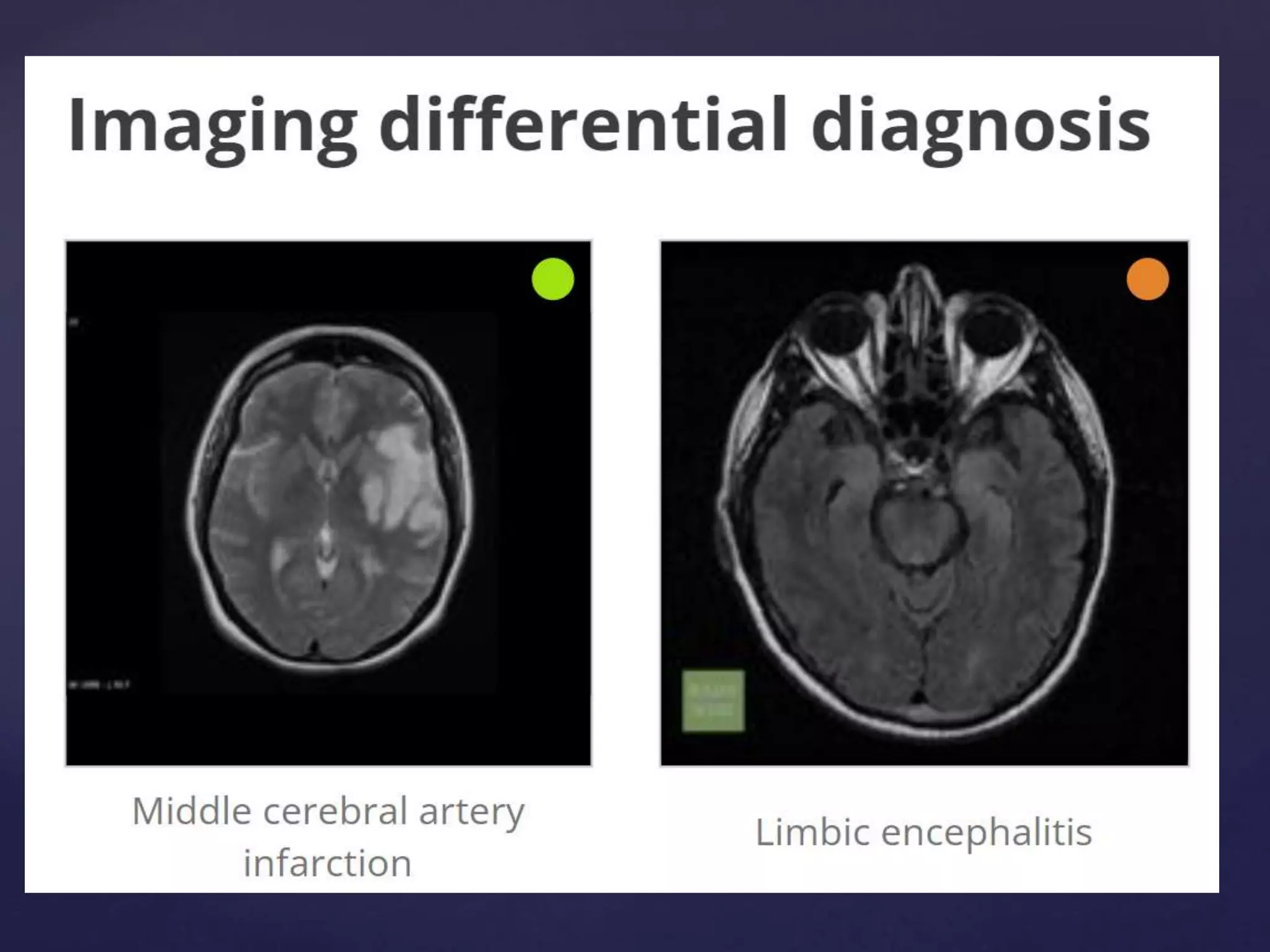
3) Herpes simplex encephalitis is a severe form caused by the herpes simplex virus. It commonly affects the temporal lobes and limbic systems bilaterally and can be diagnosed using MRI, EEG, and analysis of cerebrospinal fluid. Prompt antiv