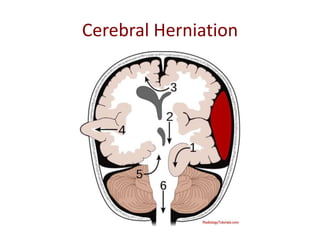
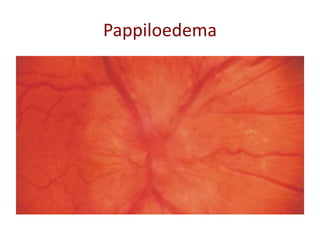
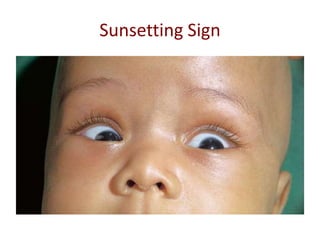
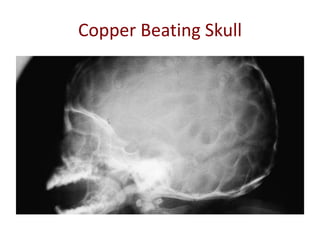
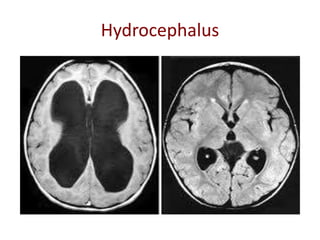
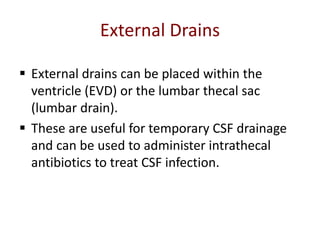
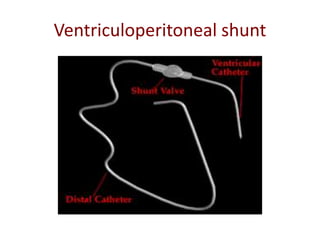
This document discusses elective neurosurgery, specifically related to raised intracranial pressure and hydrocephalus. It begins by defining normal intracranial pressure and the Monroe-Kellie hypothesis. It then describes the causes, signs, symptoms and treatments of raised intracranial pressure, including medical options like mannitol and surgical options like craniotomy. The document also discusses the physiology of cerebrospinal fluid, the pathophysiology and types of hydrocephalus, investigations for hydrocephalus, and treatments like ventriculoperitoneal shunting, external drains, and endoscopic third ventriculostomy. Complications of treatments are also outlined.