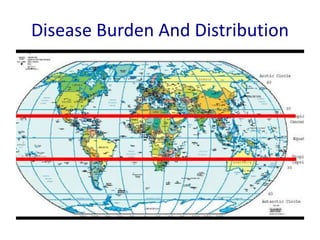
1. The document discusses common surgical conditions seen in tropical regions, including typhoid, tuberculosis, amoebiasis, ascariasis, and tropical diseases.
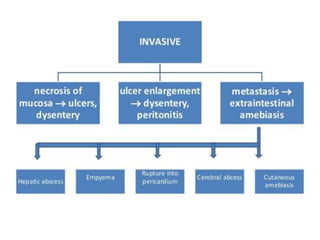
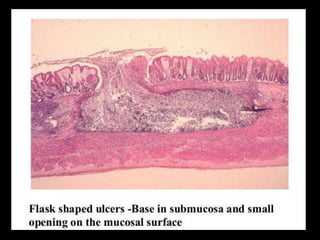
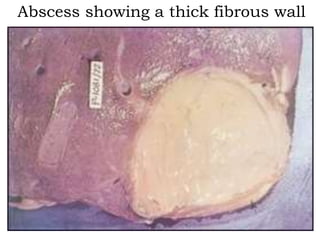
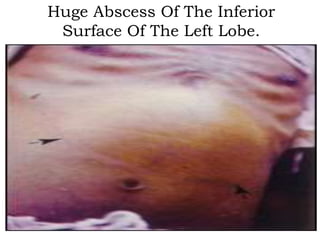
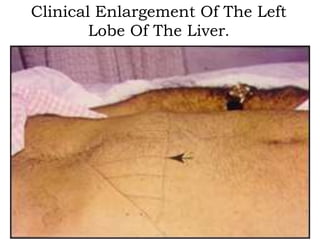
2. It provides details on the pathogenesis, clinical presentation, diagnosis, and treatment of typhoid perforation, ascariasis infection and obstruction, and amoebic liver abscess.
3. The document emphasizes that patients in tropical regions often do not seek medical help until diseases have progressed significantly, sometimes resulting in emergency presentations of conditions like typhoid perforation or ascariasis obstruction.