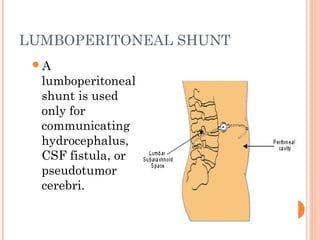
This document provides information about hydrocephalus from a seminar presentation. It defines hydrocephalus as an abnormal accumulation of cerebrospinal fluid in the brain. It describes the types of hydrocephalus, causes, clinical features, diagnosis, and treatment options like shunt surgeries. Nursing management focuses on pre-operative and post-operative care including monitoring for shunt complications, preventing infections, and educating families on home care and signs to watch for.