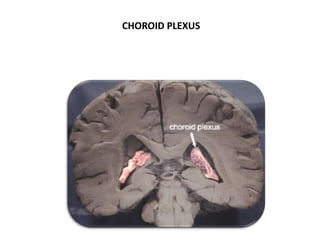
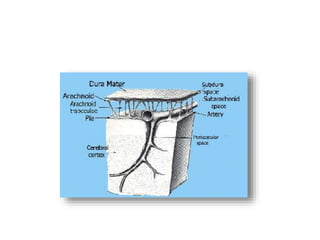
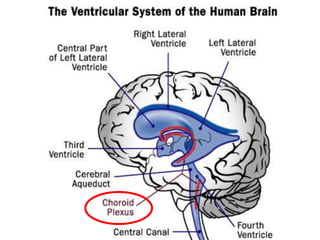
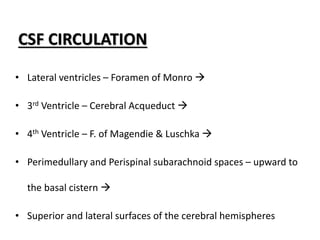
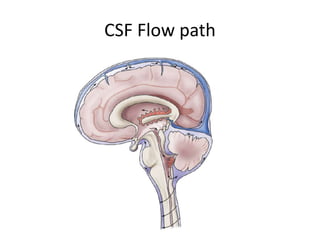
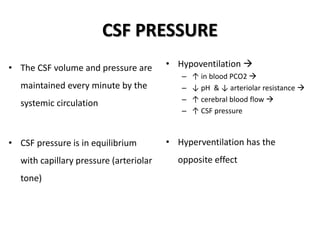
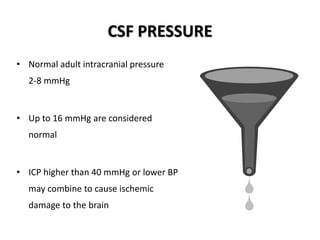
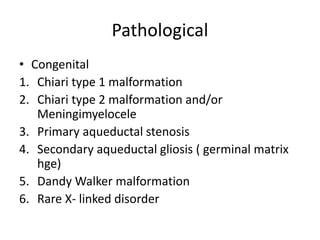
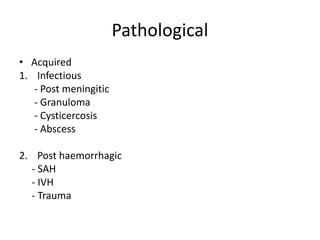
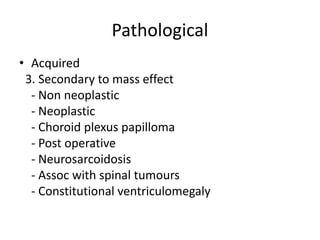
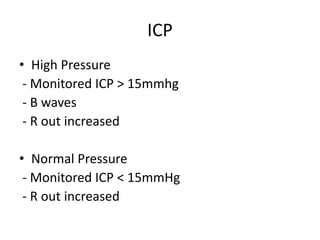
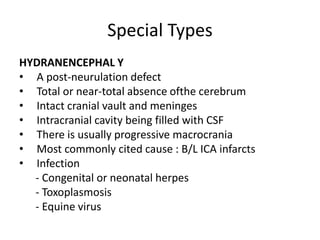
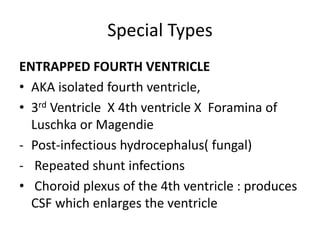
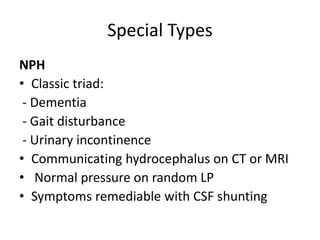
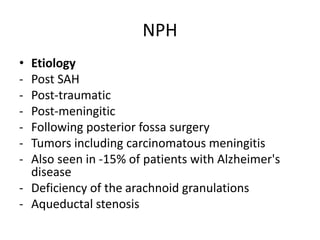
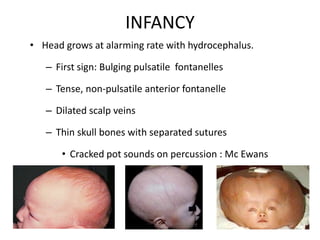
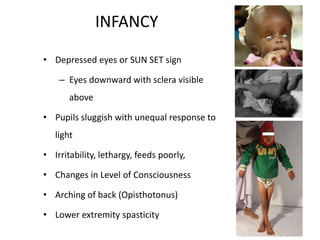
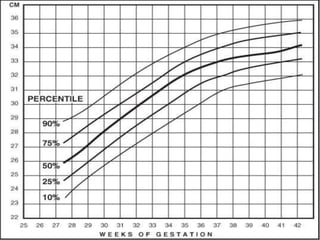
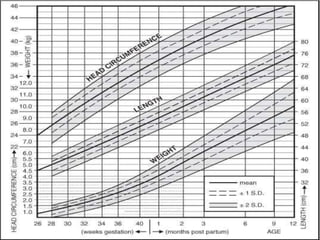
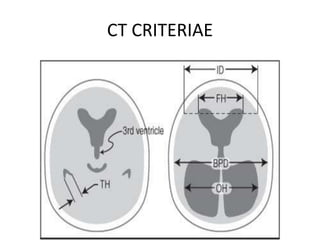
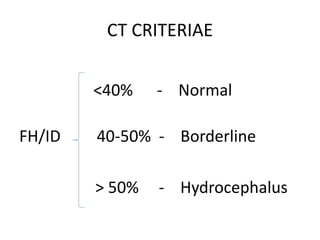
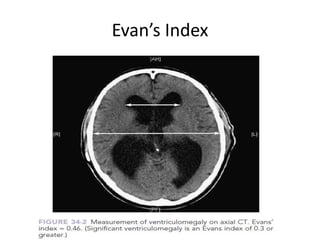
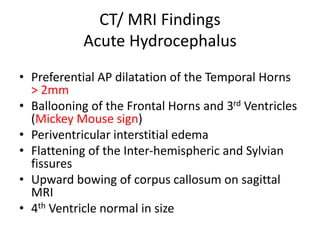
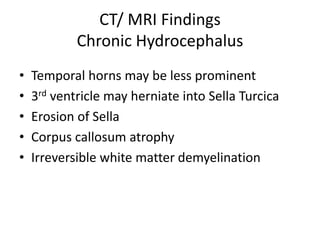
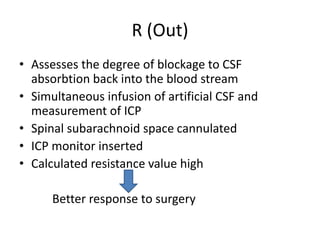
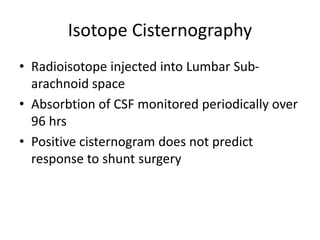
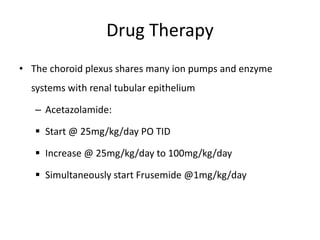
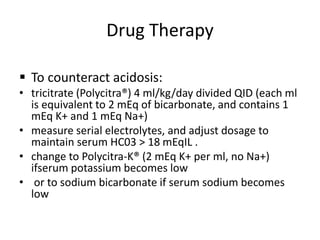
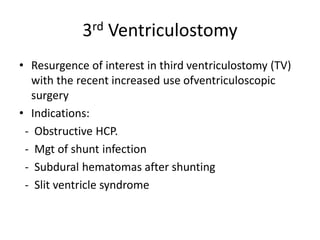
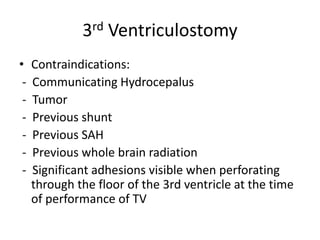
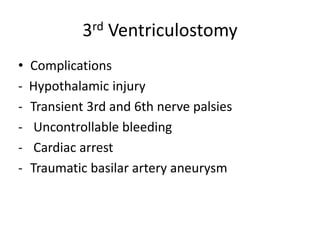
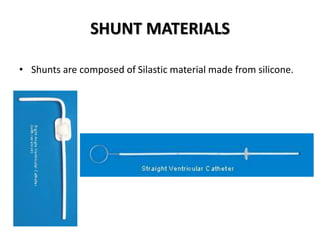
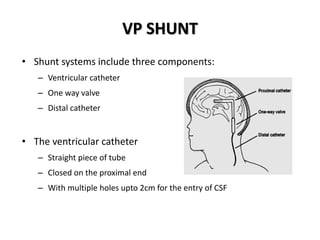
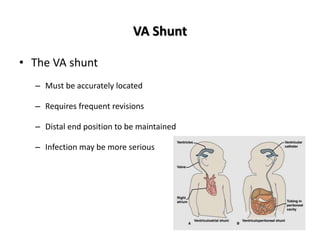
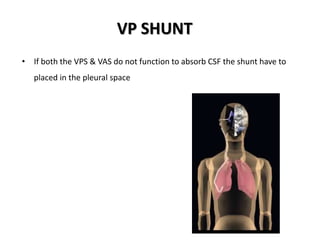
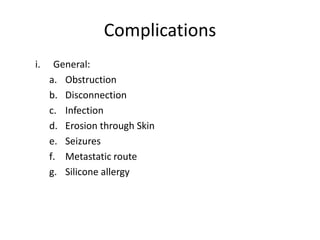
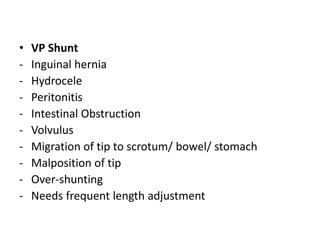
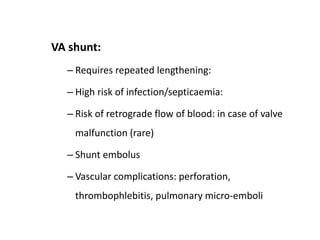
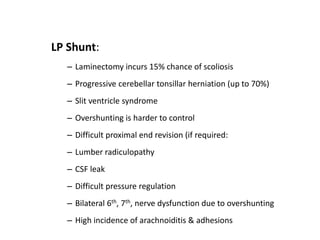
The document discusses hydrocephalus, including its evaluation, management, anatomy, physiology, and various classifications. It details cerebrospinal fluid (CSF) production, circulation, pressure, and types of hydrocephalus such as communicating and non-communicating. Additionally, it covers clinical features, diagnostic methods, and treatment options including drug therapy and surgical interventions like shunt placement.