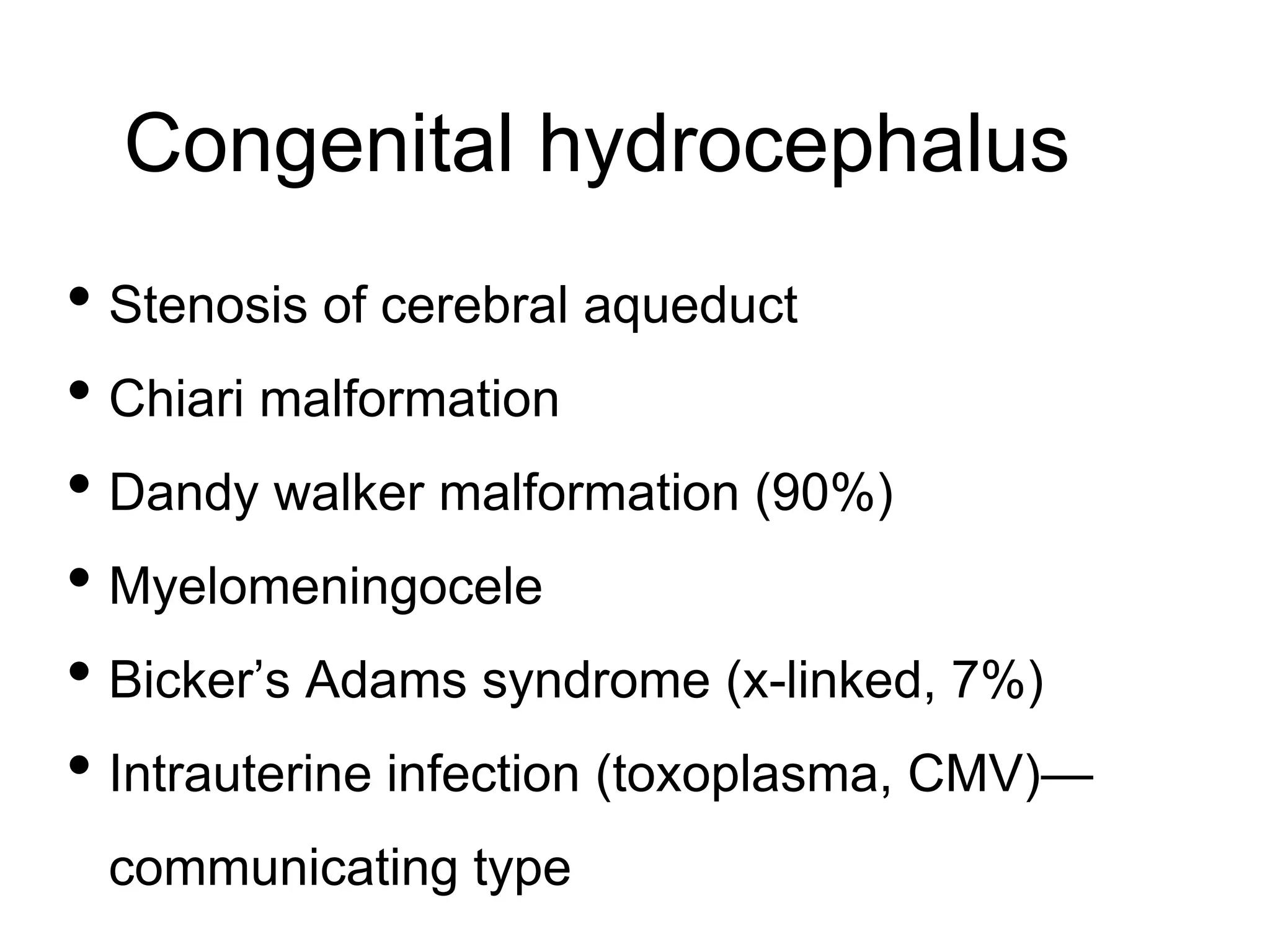
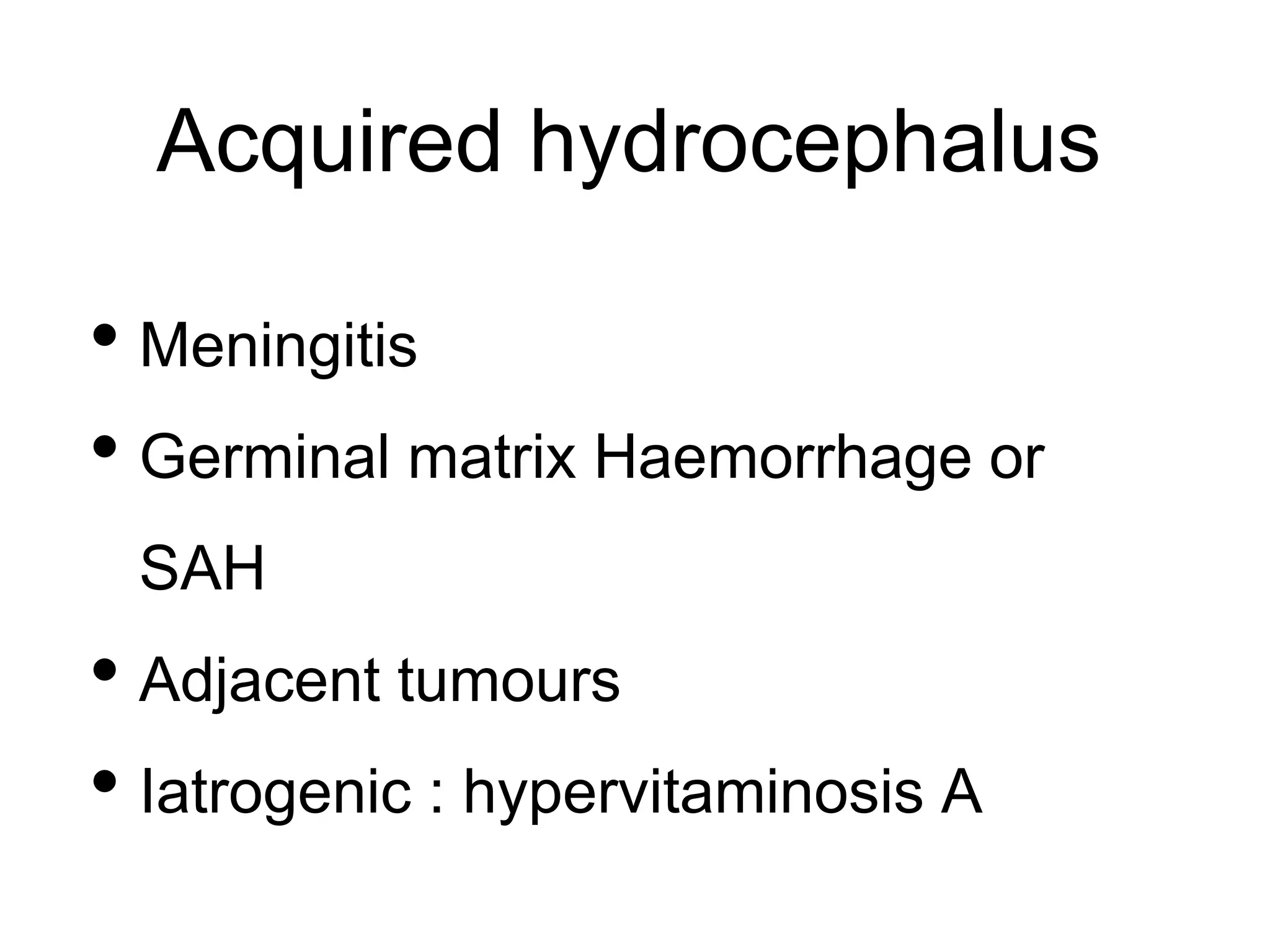
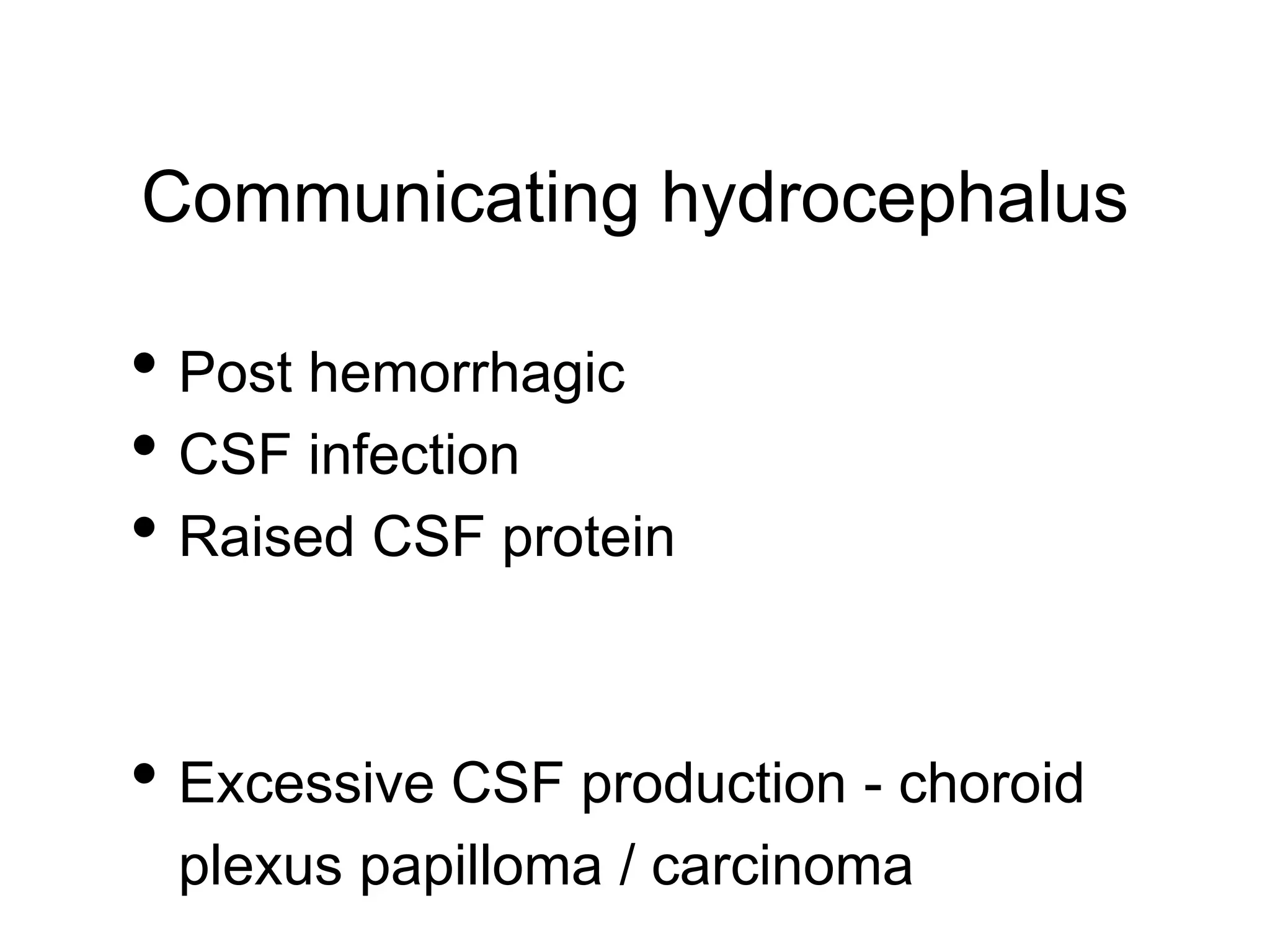
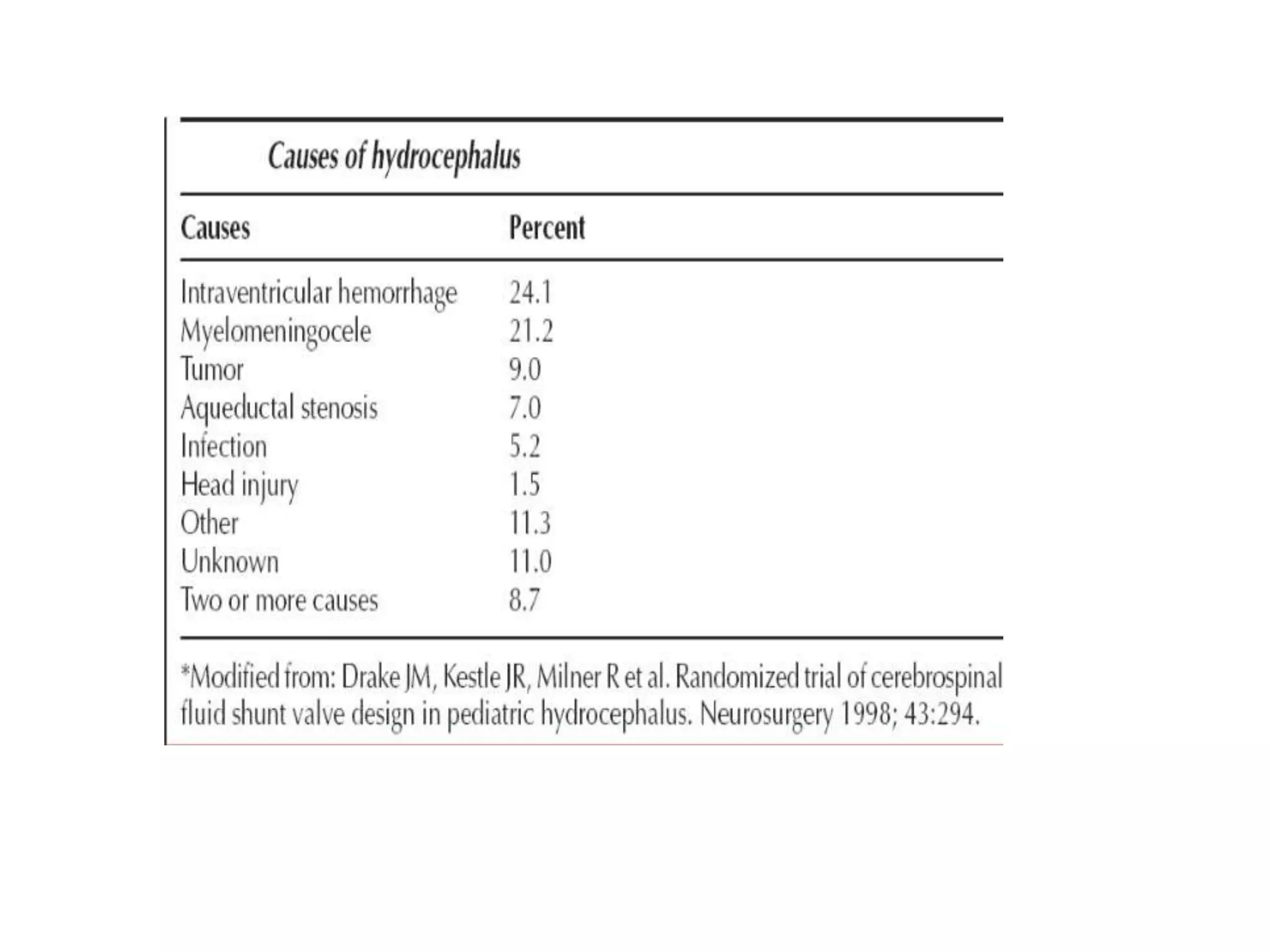
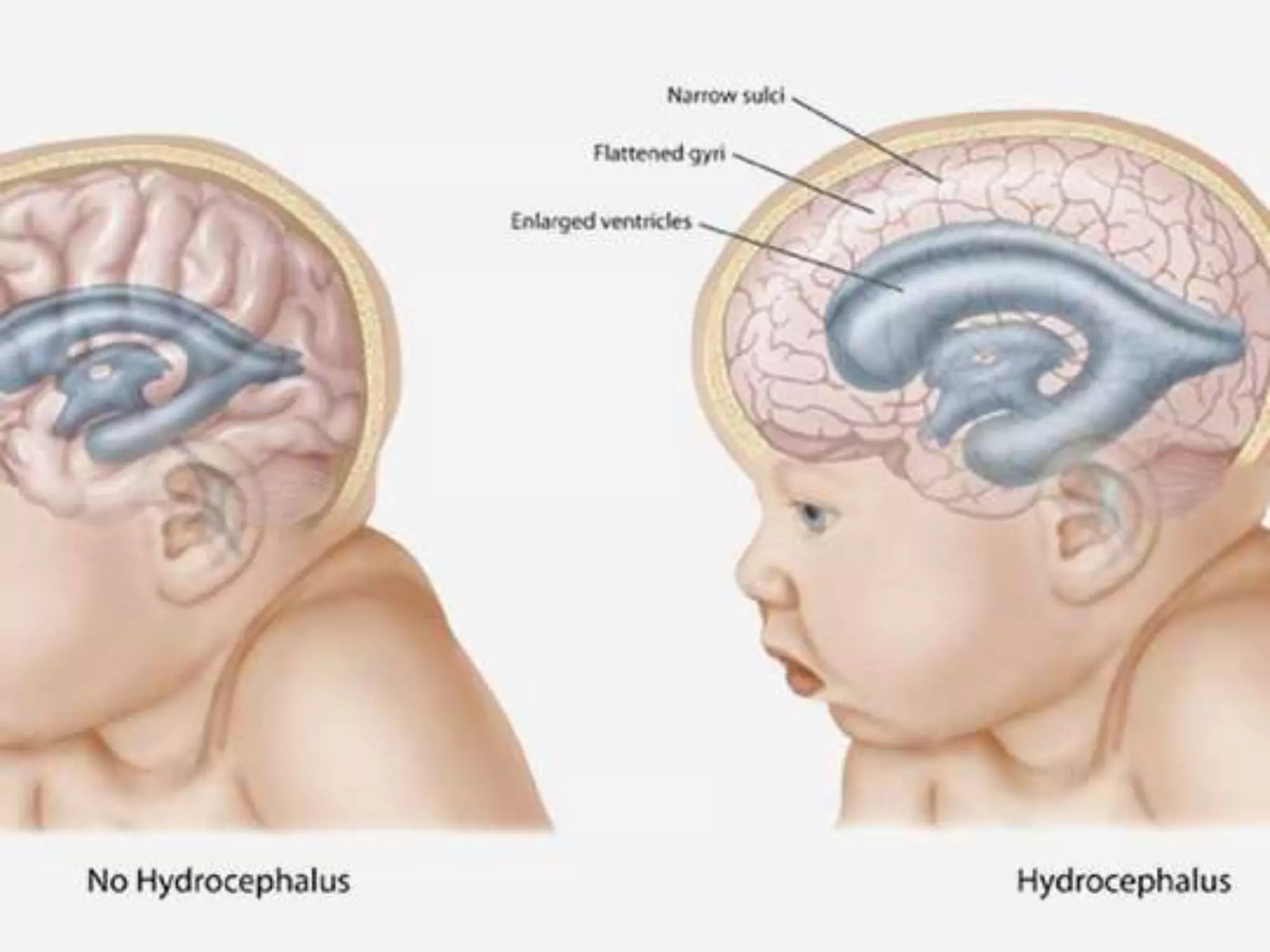
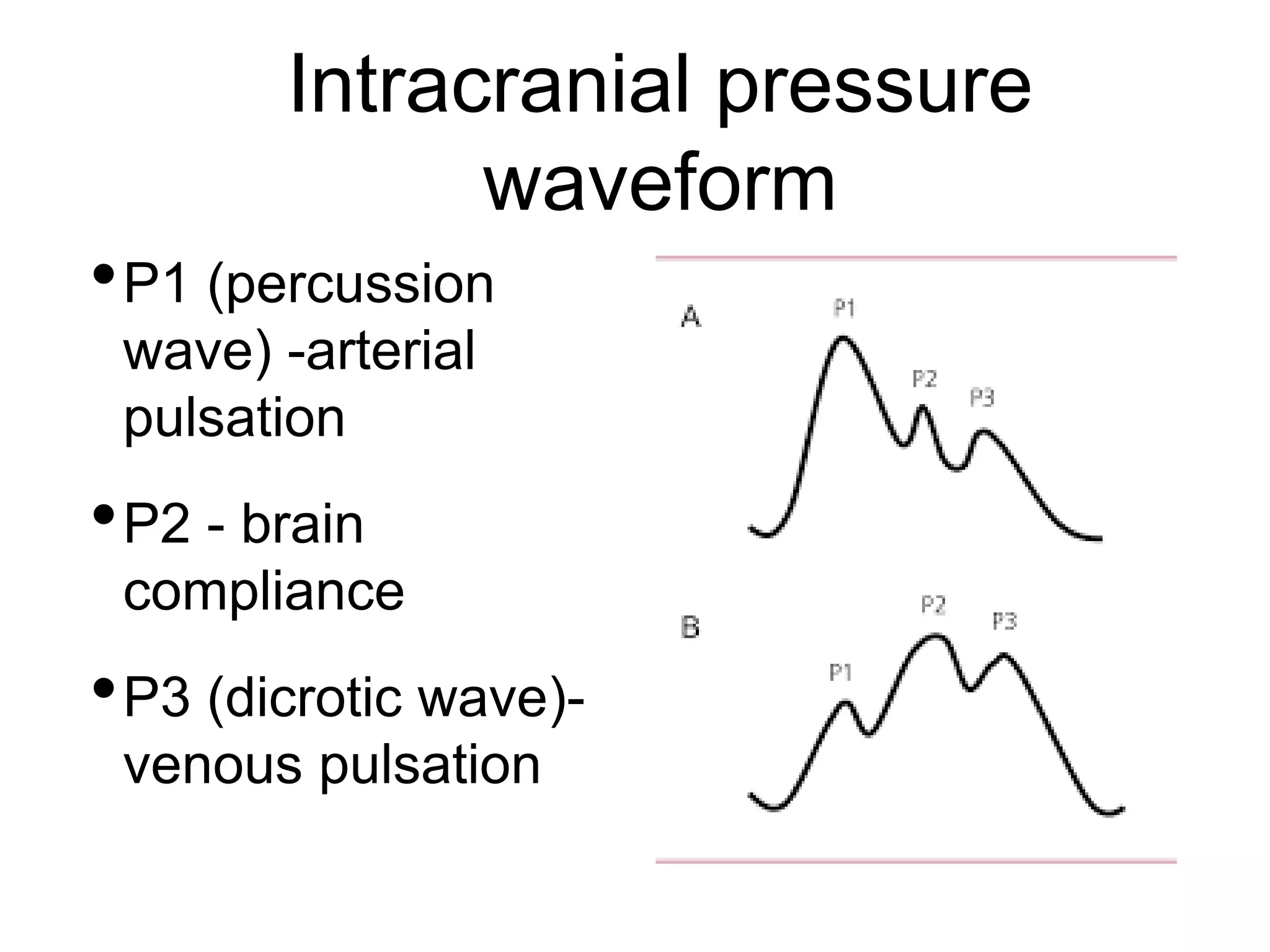
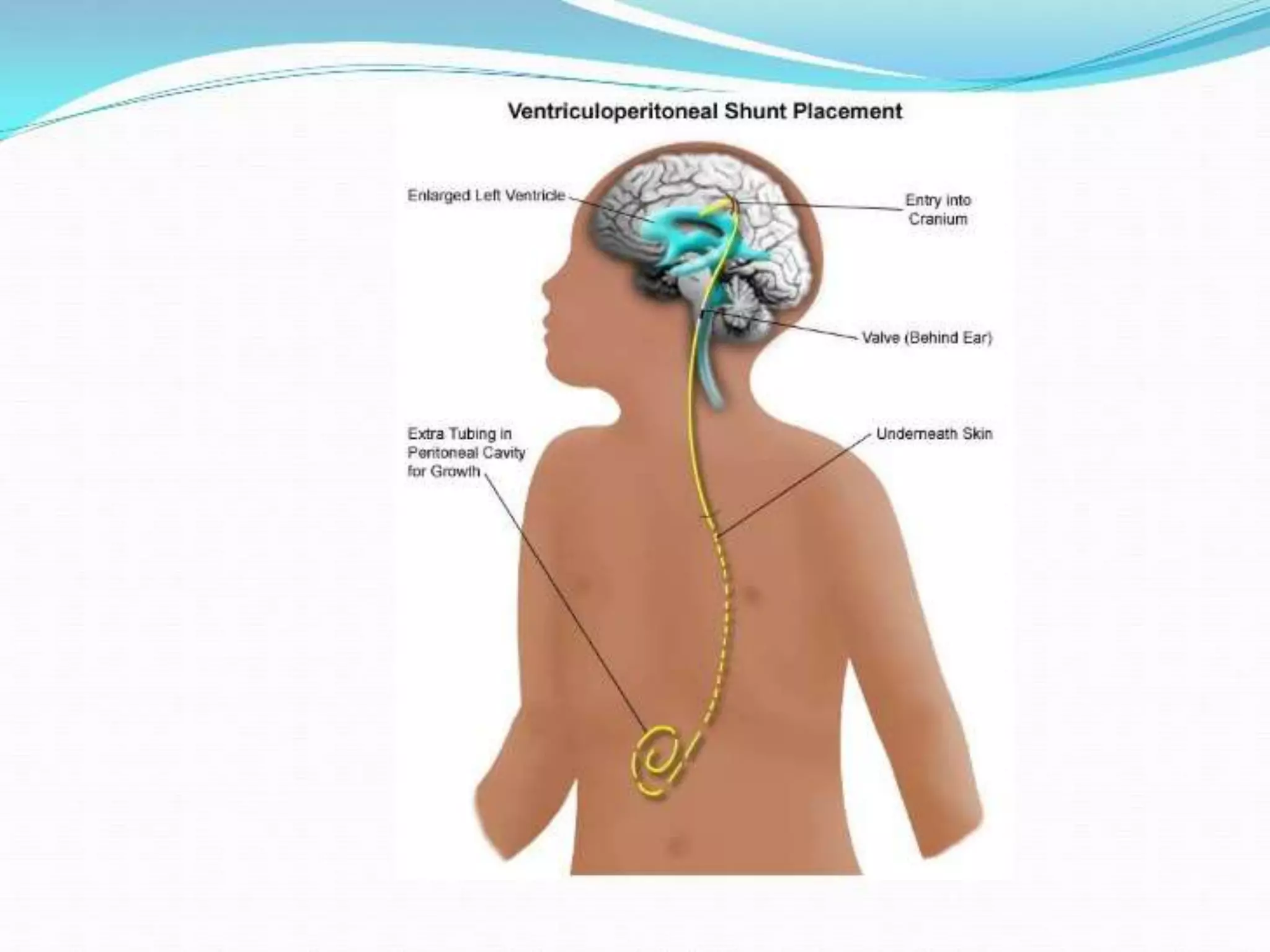
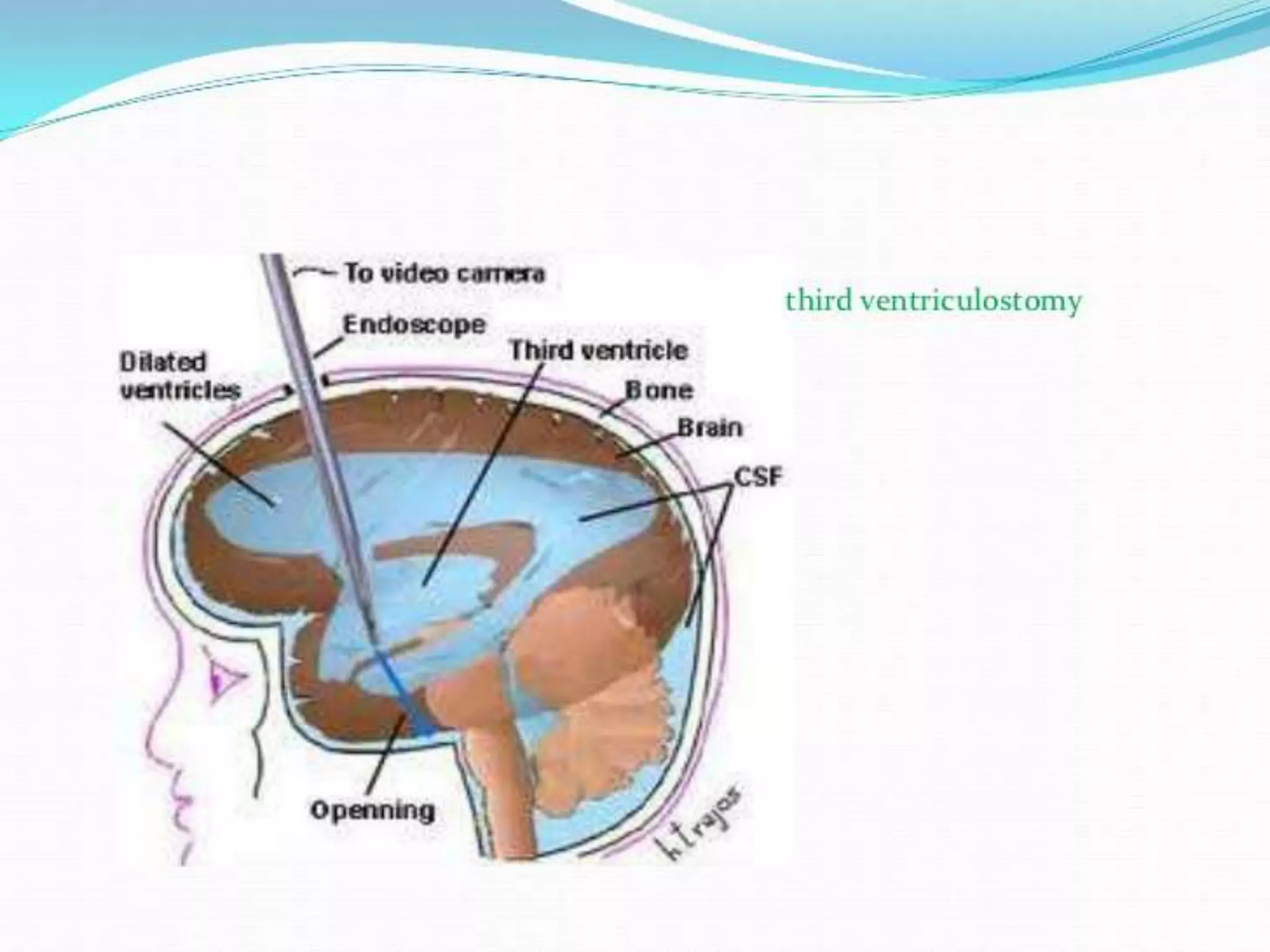
This document summarizes a seminar presentation on hydrocephalus. It defines hydrocephalus as an increase in CSF volume with ventricular enlargement. It describes the physiology of CSF circulation and different types of hydrocephalus including obstructive, communicating, congenital and acquired. Clinical presentations and investigations are discussed. Treatment options include temporary external ventricular drainage, VP shunt placement, and endoscopic third ventriculostomy. Complications of shunt surgery and new treatment modalities are also summarized.