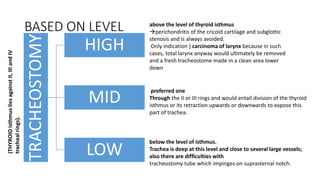
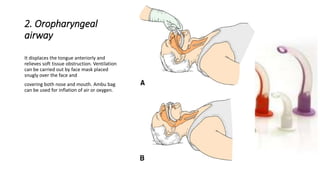
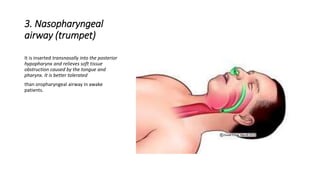
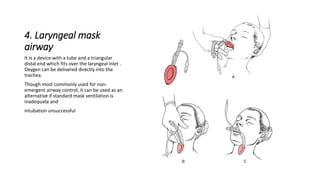
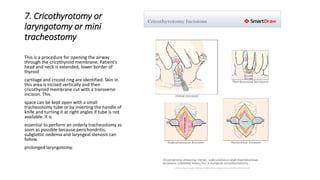
Tracheostomy is a surgical procedure that creates an opening in the anterior wall of the trachea and connects it to the skin surface, allowing for an alternative airway. It has several functions, including improving breathing, protecting the airways, and permitting removal of secretions. Indications for tracheostomy include respiratory obstruction, retained secretions, and respiratory insufficiency. Complications can occur during or after the procedure and with prolonged use of a tracheostomy tube. Alternative airway management techniques can be used to relieve an obstruction prior to an emergency tracheostomy.