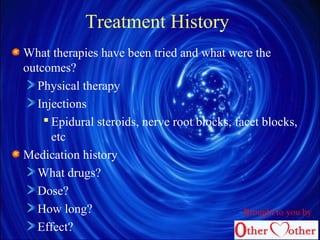
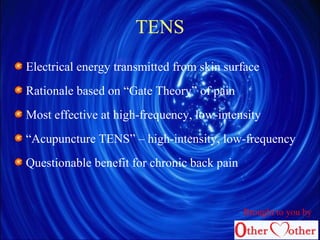
This document provides an overview of failed back surgery syndrome (FBSS), including its diagnosis, evaluation, and treatment. It defines FBSS as continued back and/or extremity pain following one or more spinal surgeries. Common causes of FBSS include deconditioning, psychosocial factors, and surgical complications. The evaluation of FBSS involves a detailed pain history, physical exam, imaging, and may include diagnostic blocks. Treatment is multidisciplinary and aims to improve function through physical therapy, psychological treatments, and pain management with medications, injections, or devices.