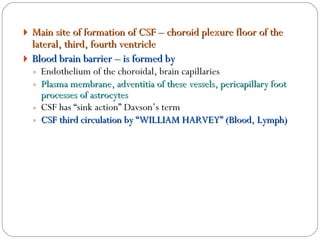
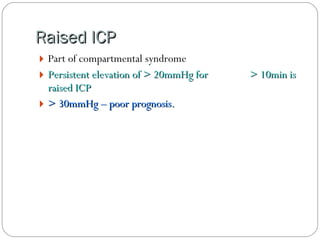
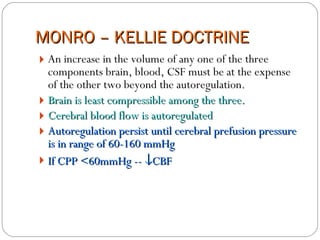
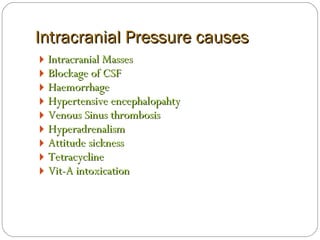
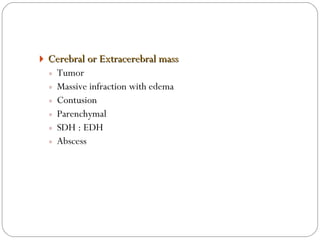
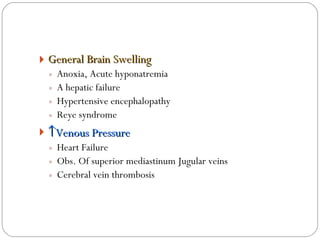
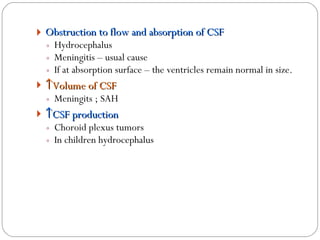
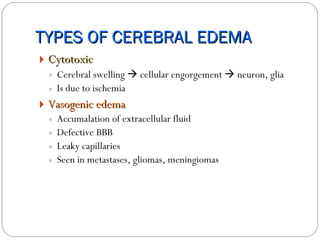
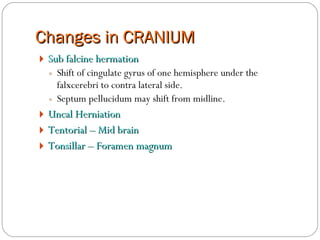
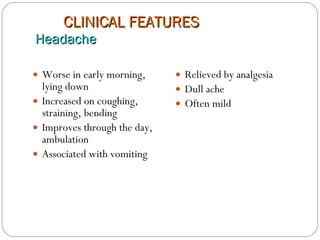
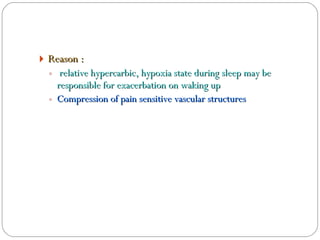
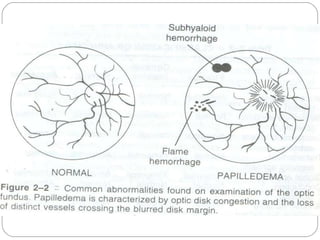
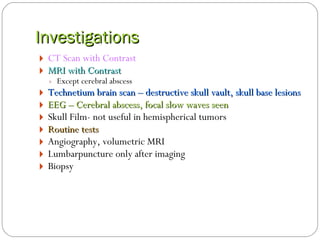
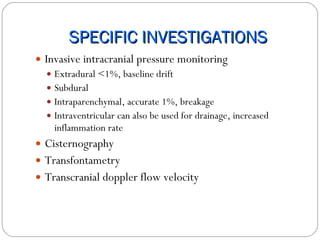
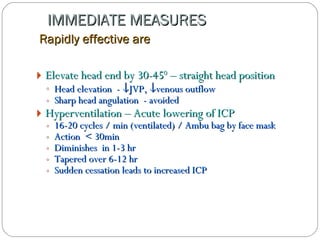
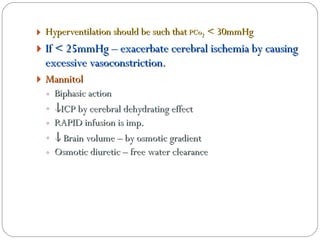
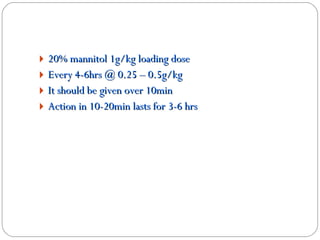
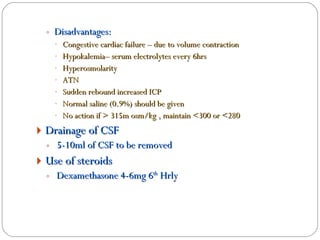
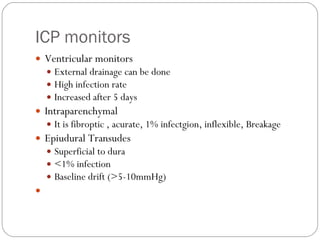
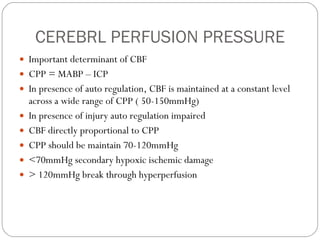
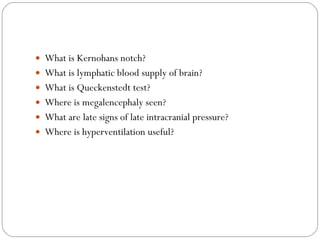
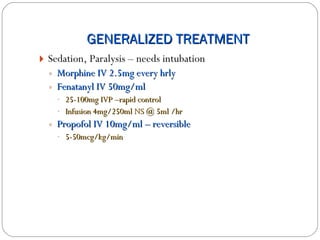
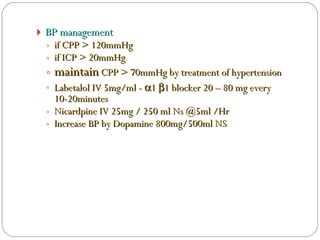
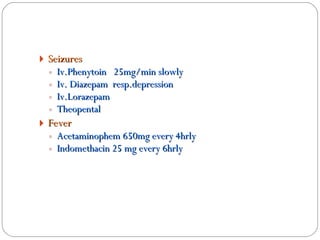
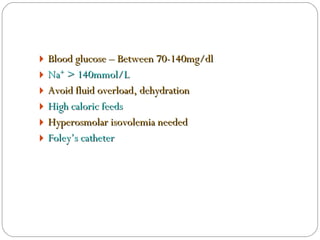
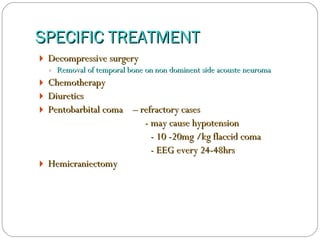
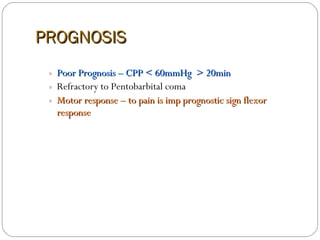
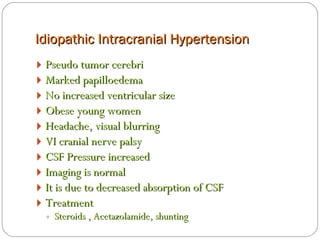
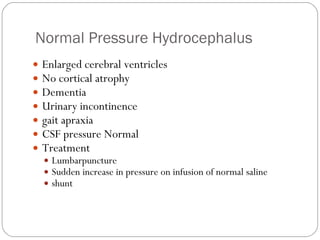
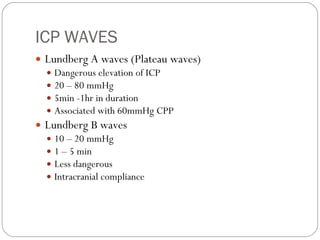
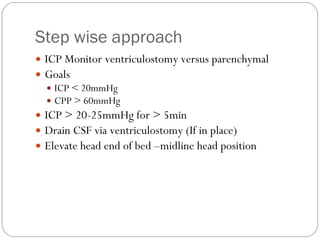
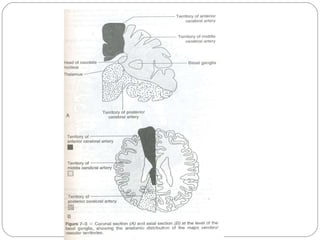
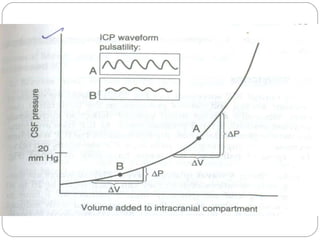
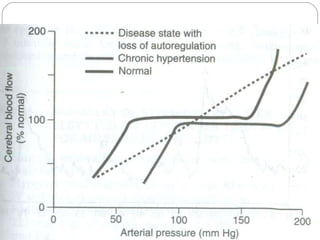
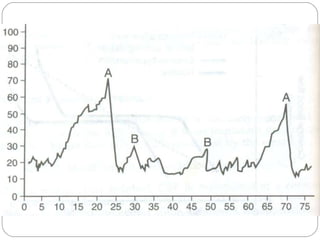
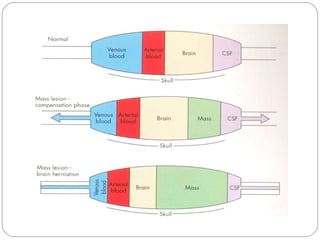
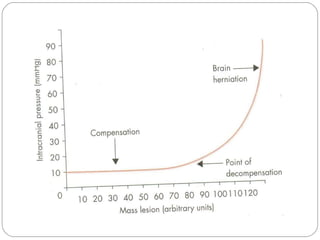
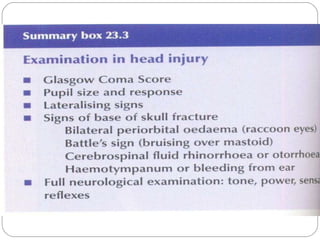
The document discusses intracranial pressure (ICP), providing definitions and normal values. It describes cerebrospinal fluid (CSF) and autoregulation of cerebral blood flow. It covers evaluation of raised ICP including Monro-Kellie doctrine, Cushing's triad, and changes in the cranium. It discusses types of cerebral edema and causes of raised ICP. Clinical features, investigations, and general treatment protocols are outlined. Specific conditions like normal pressure hydrocephalus and idiopathic intracranial hypertension are briefly mentioned. Prognosis is also covered.