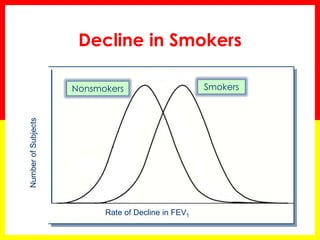
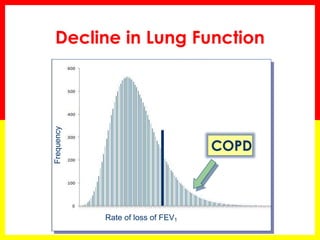
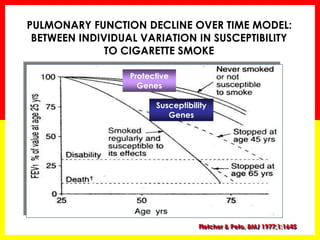
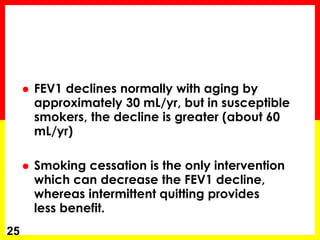
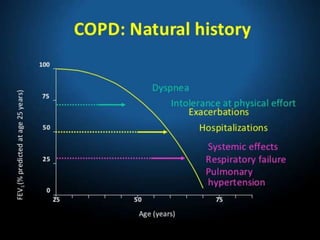
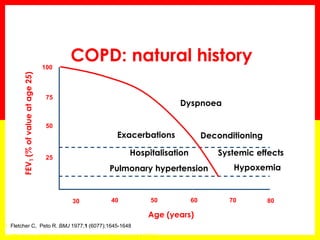
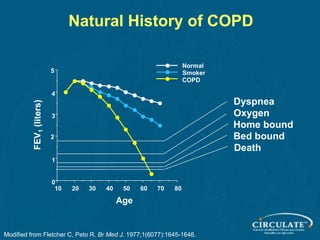
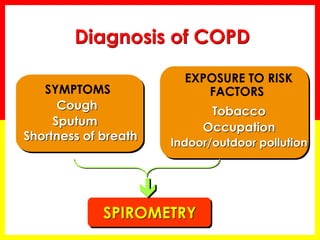
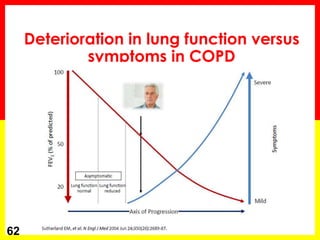
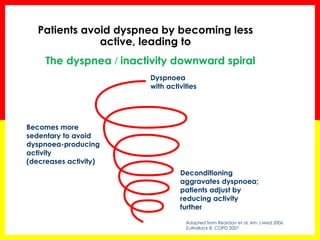
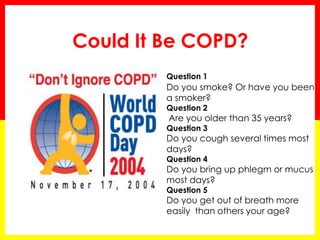
Chronic obstructive pulmonary disease (COPD) has a variable natural history. It is generally a progressive disease if exposure to noxious agents like cigarette smoke continues. While not all smokers develop clinically significant COPD, those who do experience an accelerated decline in lung function of about 60 mL/yr compared to 30 mL/yr in normal aging. Stopping smoking can slow this progression. The cardinal symptoms of COPD are dyspnea, chronic cough, and sputum production. Dyspnea is usually progressive and becomes persistent with minimal exertion as the disease worsens.