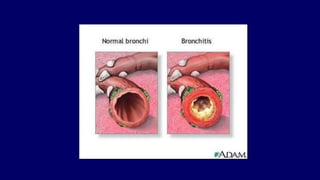
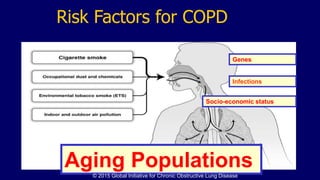
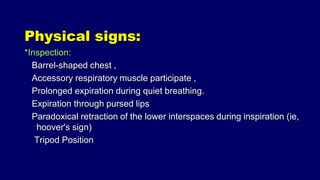
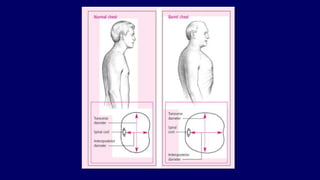
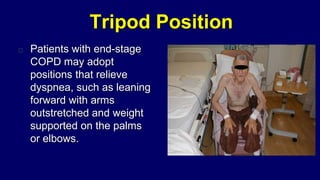
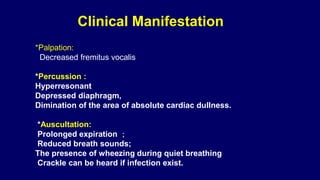
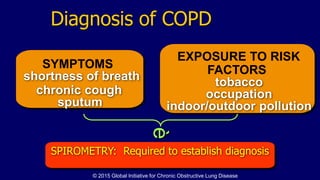
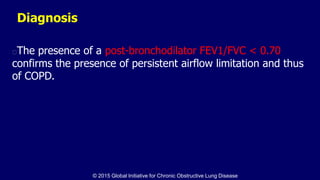
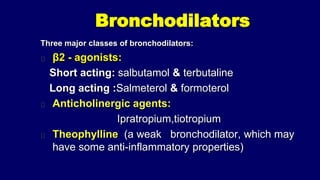
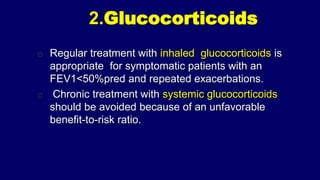
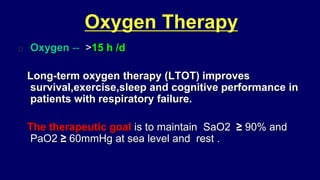
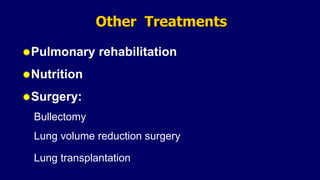
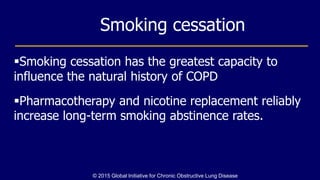
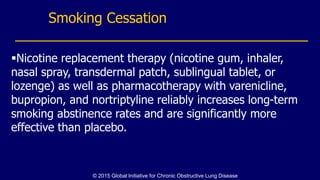
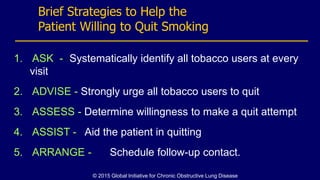
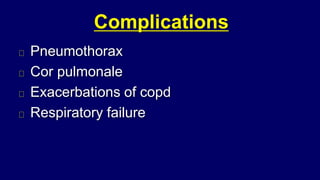
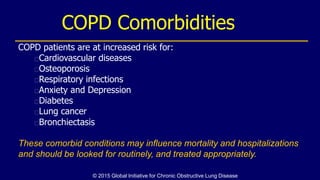
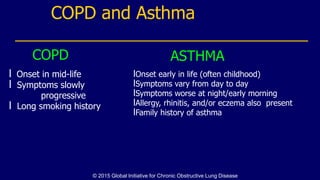
Chronic obstructive pulmonary disease (COPD) is a preventable and treatable condition characterized by progressive airflow limitation and is a leading cause of morbidity and mortality. Common risk factors include smoking, genetics, and environmental pollutants, with symptoms such as chronic cough, dyspnea, and sputum production. Management focuses on bronchodilators, glucocorticoids, and lifestyle changes including smoking cessation to improve quality of life and reduce exacerbations.