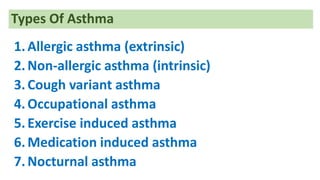
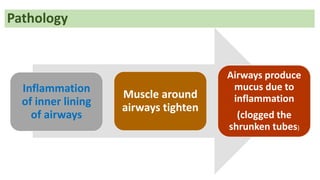
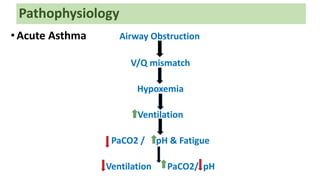
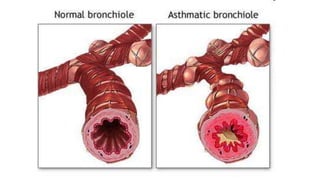
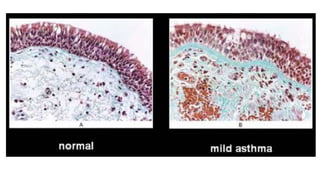
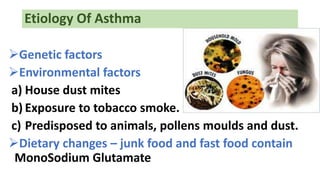
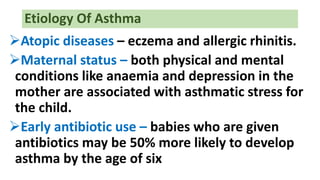
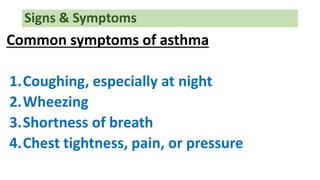
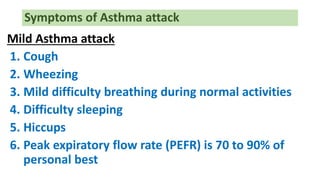
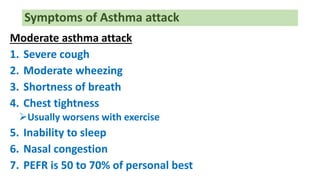
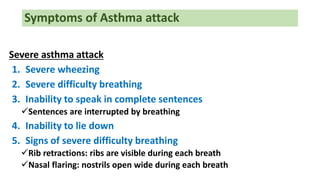
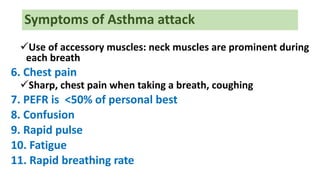
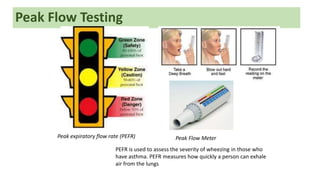
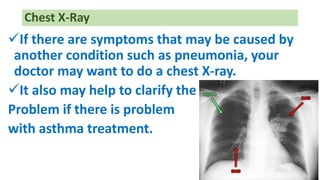
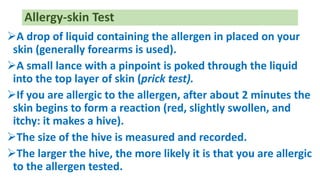
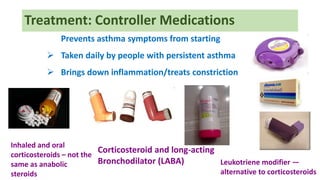
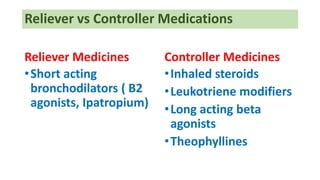
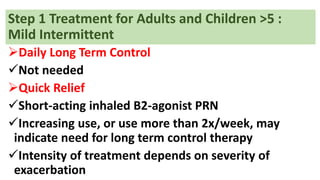
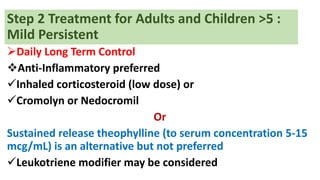
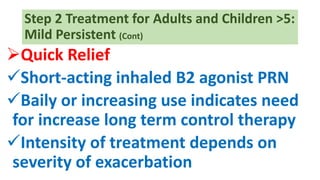
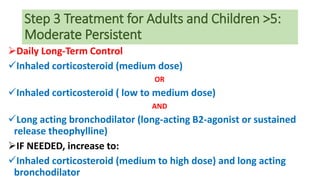
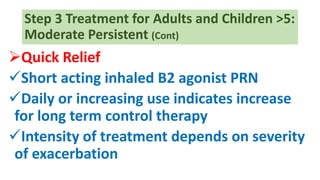
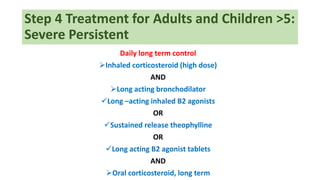
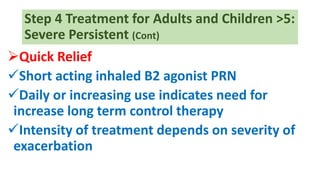
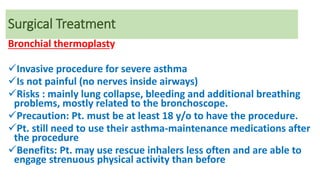
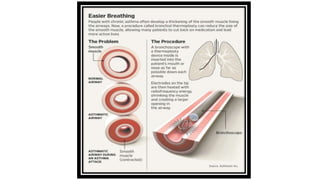
This document provides information on asthma, including its definition, types, pathophysiology, etiology, symptoms, diagnosis, and treatment. Asthma is defined as a chronic inflammatory disease of the airways characterized by variable airflow obstruction and airway hyperresponsiveness. It discusses the different types of asthma including allergic, non-allergic, cough variant, occupational, and exercise-induced asthma. Treatment involves both controller medications to reduce inflammation and reliver medications for acute symptoms. Treatment is escalated in steps based on asthma severity and control.