Embed presentation
Downloaded 175 times
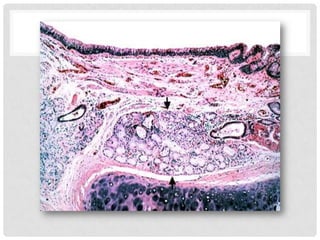
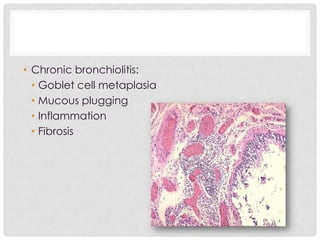
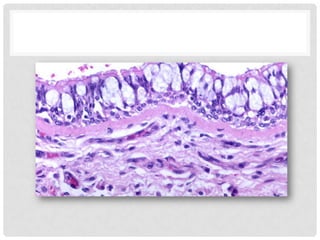
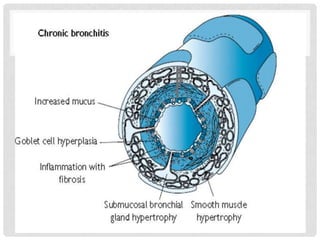
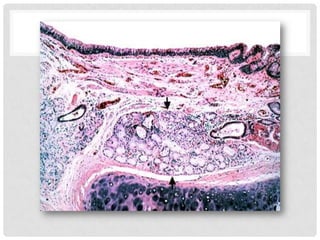
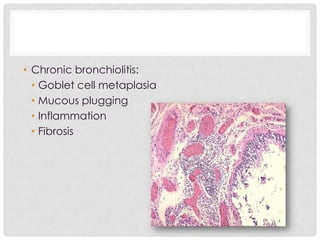
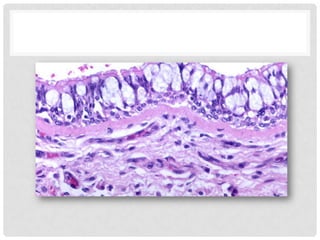
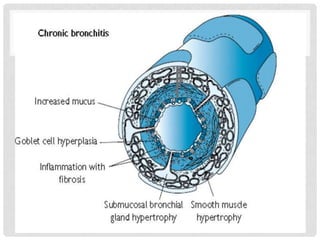
Shahd Alali has chronic bronchitis, characterized by a chronic cough lasting over 2 years. Chronic bronchitis is common among smokers and is caused by smoking as well as air pollutants. It involves hypertrophy of the bronchial mucus glands leading to hypersecretion of mucus and inflammation in the large airways. On morphology, the large airways appear hyperemic, swollen, and covered in mucus secretions with increased goblet cells and inflammatory cells in the trachea and bronchi. Clinical features include a prominent cough producing sputum, cyanosis, increased risk of infection, and dyspnea.