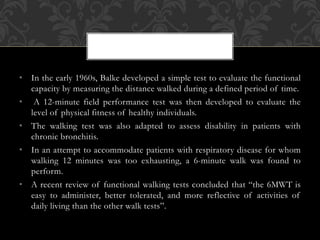
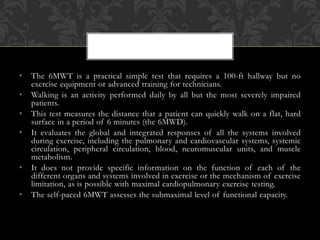
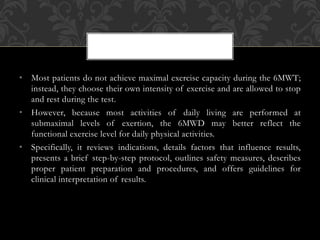
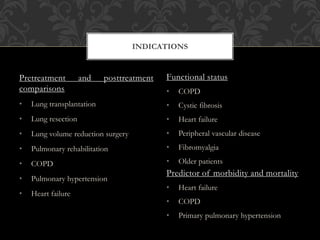
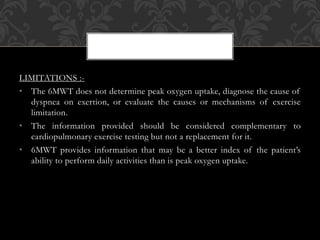
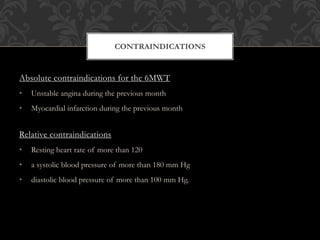
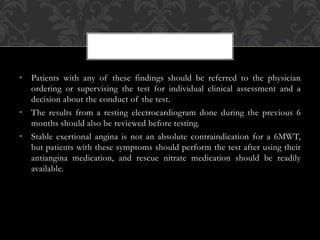
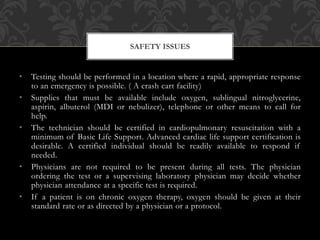
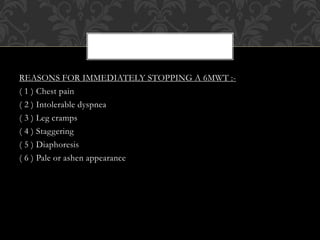
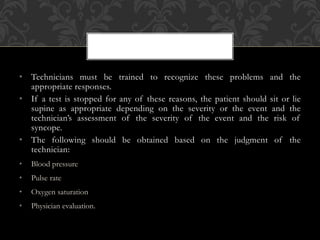
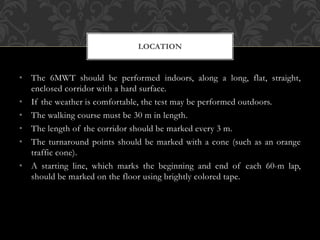
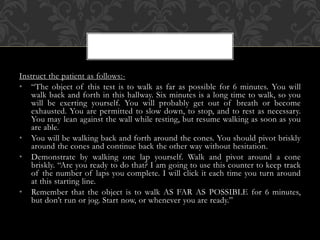
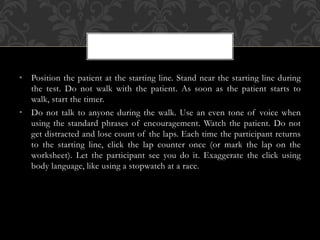
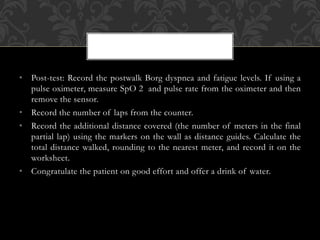
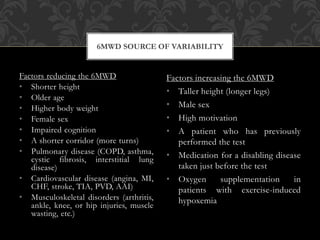
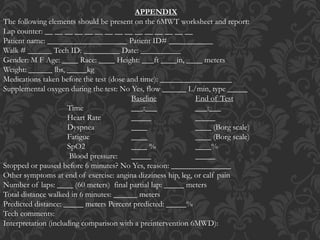
The document outlines the 6-minute walk test (6MWT), a simple and practical method for assessing functional exercise capacity, particularly in patients with chronic lung and heart diseases. It details the test's protocol, indications, limitations, and safety measures, emphasizing its role as a predictor of morbidity and mortality. The test is well-tolerated and reflects daily activity levels, making it a valuable tool for evaluating patients' functional status and responses to medical interventions.