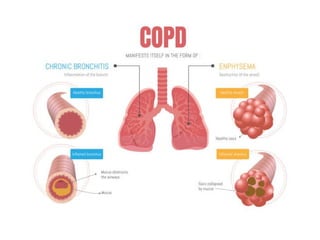
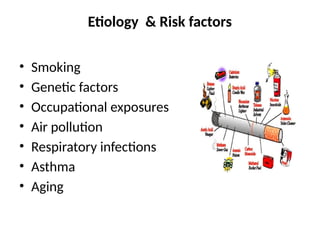
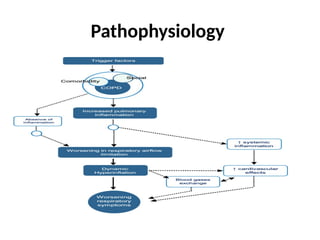
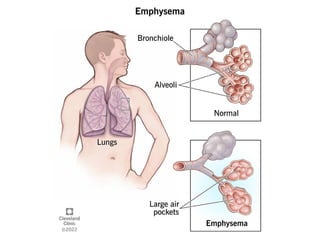
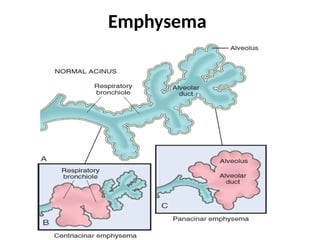
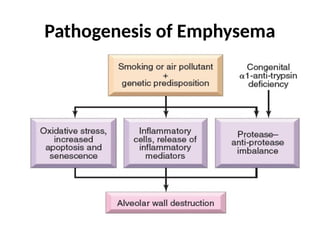
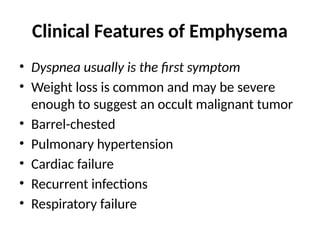
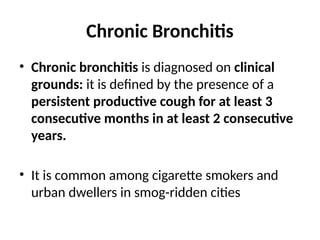
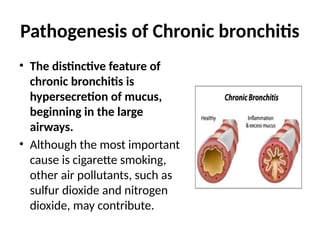
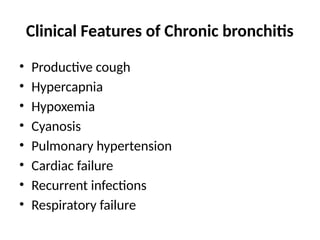
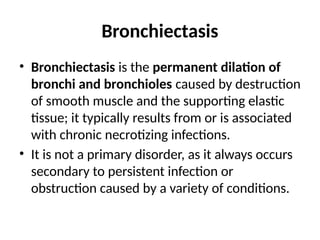
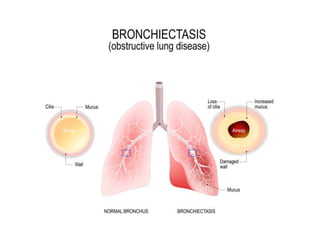
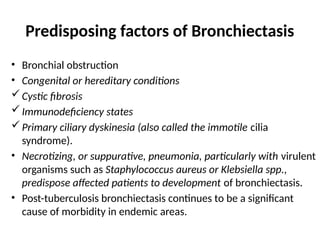
The document provides an overview of Chronic Obstructive Pulmonary Disease (COPD), detailing its definition, etiology, pathophysiology, and clinical presentations including emphysema, chronic bronchitis, and bronchiectasis. It outlines common symptoms, risk factors, and diagnostic investigations, as well as management strategies for controlling the disease. It emphasizes the lack of a cure but highlights the importance of treatment options such as smoking cessation, medications, and pulmonary rehabilitation.