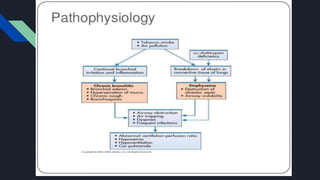
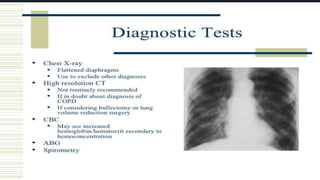
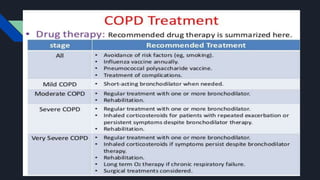
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease characterized by limited airflow in the lungs. It includes conditions like emphysema and chronic bronchitis. In COPD, the airways and air sacs are damaged, making it difficult to breathe out fully. The damage can be caused by smoking, air pollution, dust, or genetic factors. Symptoms include increased shortness of breath, cough, wheezing and tightness in the chest. Treatment focuses on reducing symptoms through bronchodilators, antibiotics, steroids, and quitting smoking to prevent further damage.