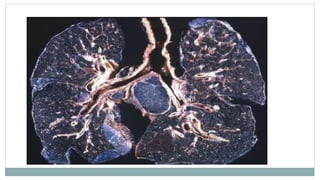
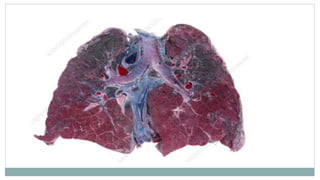
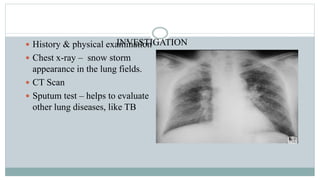
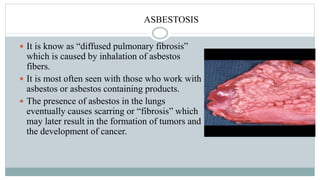
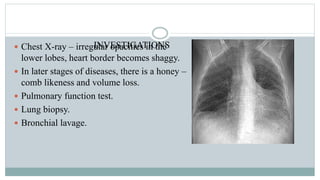
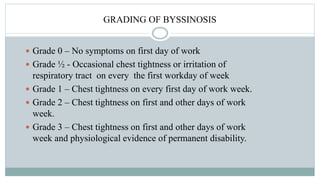
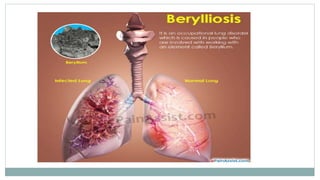
Occupational lung diseases are caused by exposure to dusts, chemicals, or other agents in the workplace. Some examples described in the document include silicosis from inhaling silica dust, asbestosis from asbestos exposure, byssinosis from cotton dust, and farmer's lung caused by mold exposure. Symptoms vary but often include cough, shortness of breath, and lung impairment. Diagnosis involves exams, imaging, and pulmonary function tests. Treatment focuses on removing the causal exposure and managing symptoms, though many occupational lung diseases have no cure.