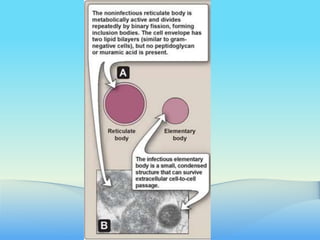
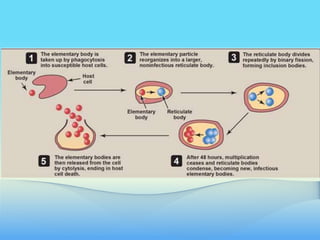
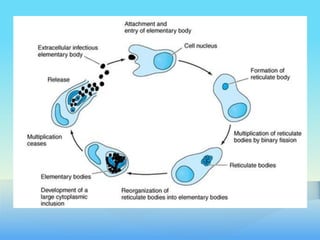
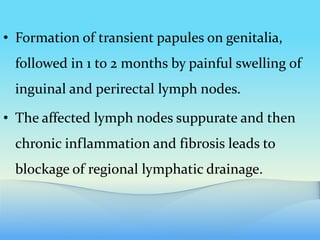
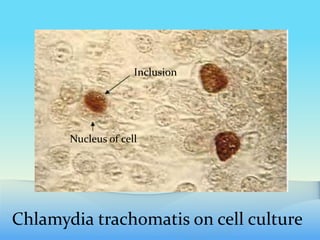
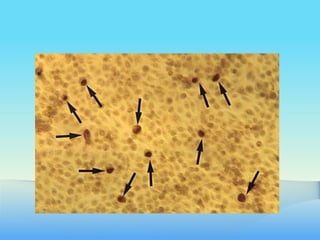
Chlamydiae are obligate intracellular pathogens, with three key human species: Chlamydia trachomatis, Chlamydophila psittaci, and Chlamydophila pneumoniae, each causing different diseases like STDs and pneumonia. C. trachomatis, the most common STD pathogen, presents in multiple serotypes associated with conditions such as trachoma and lymphogranuloma venereum. Diagnosis typically involves detecting intracytoplasmic inclusion bodies or antigens in specimens, with treatment options including tetracyclines and macrolides.