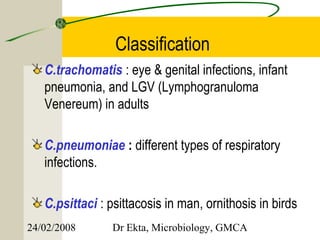
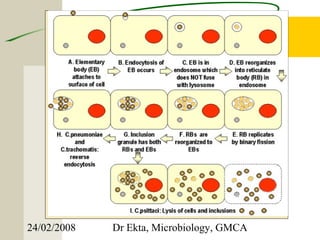
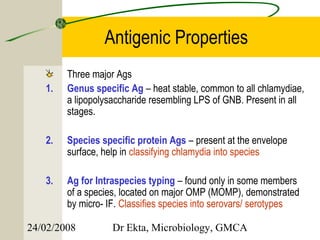
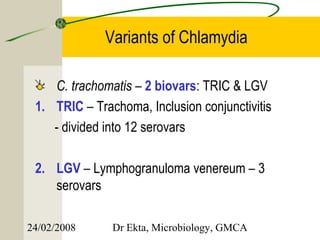
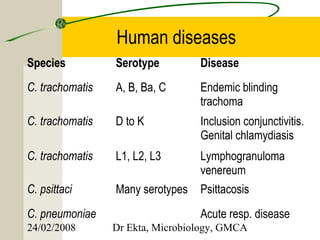
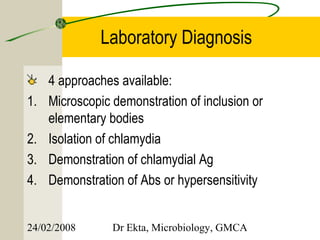
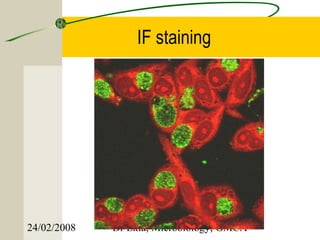
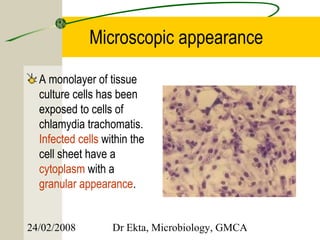
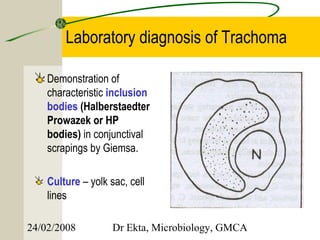
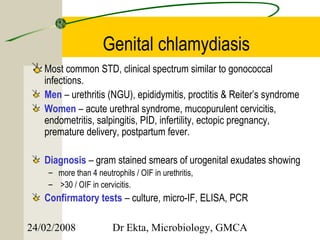
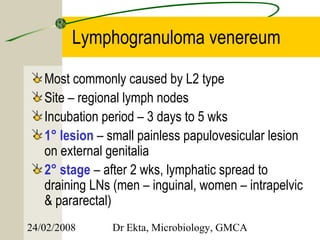
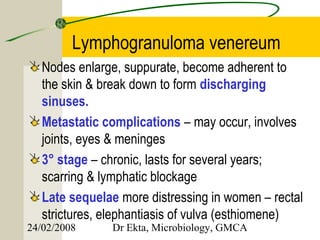
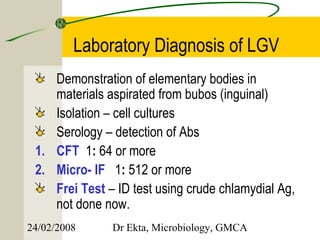
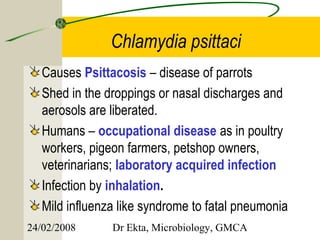
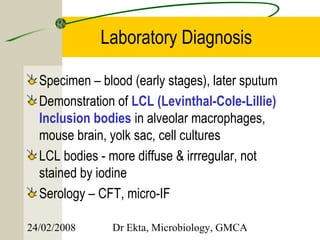
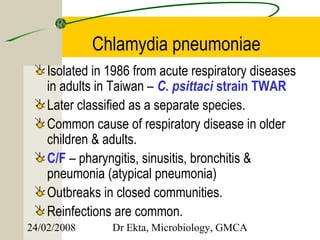
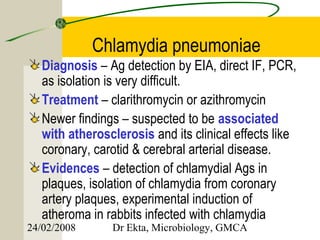
This document discusses Chlamydia, an obligate intracellular parasite. It describes the four species that infect humans (C. trachomatis, C. pneumoniae, C. psittaci, C. pecorum) and their associated diseases. C. trachomatis causes trachoma, inclusion conjunctivitis, infant pneumonia, and genital infections like lymphogranuloma venereum. The life cycle and laboratory diagnosis of Chlamydia species are also summarized.