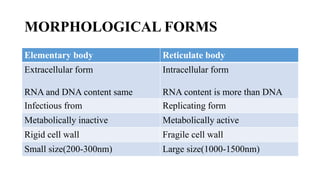
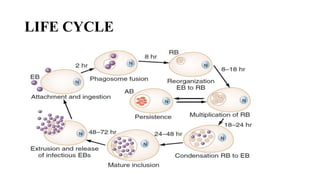
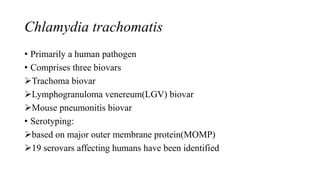
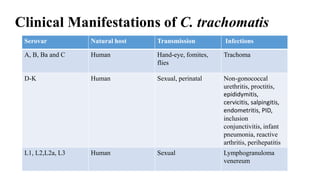
This document discusses human chlamydiasis, which is caused by intracellular bacteria from the Chlamydia and Chlamydophila genera. It describes the classification, morphological forms, antigenic structure, and life cycle of these bacteria. It then focuses on Chlamydia trachomatis, covering its serovars and the infections they cause like trachoma, lymphogranuloma venereum, and pneumonia. Diagnostic testing and treatment options for various chlamydial infections are also outlined.