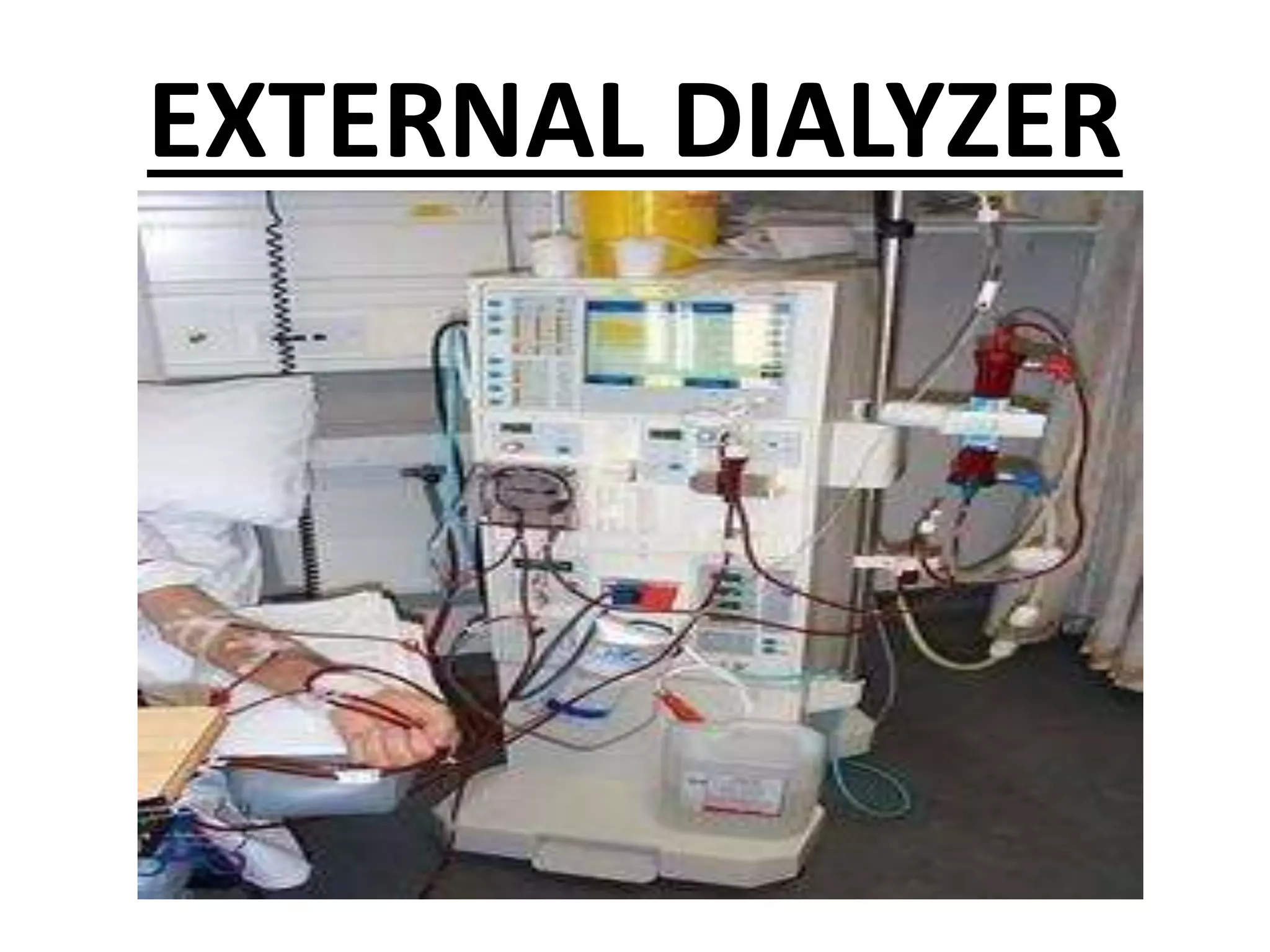
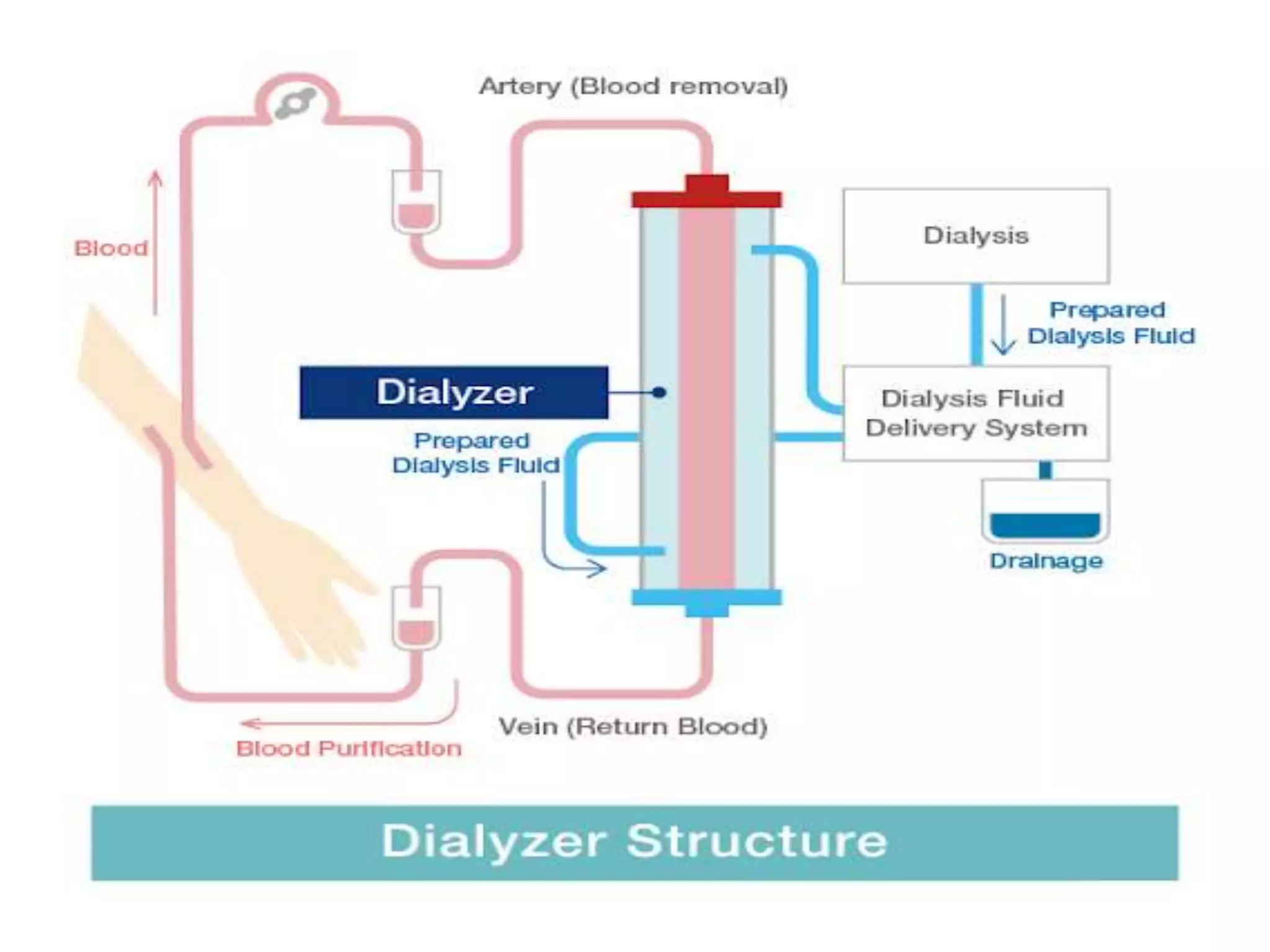
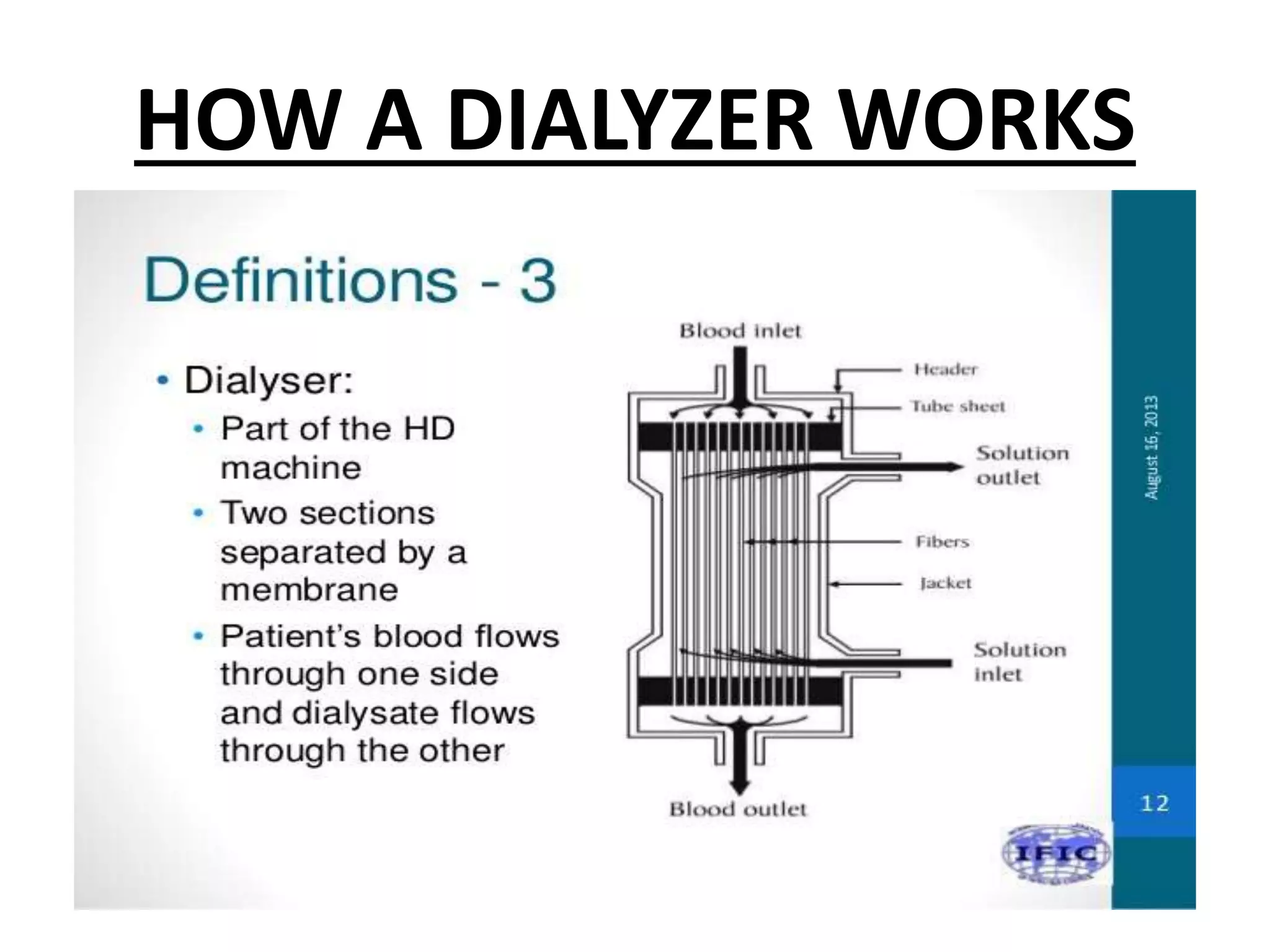
A dialyzer is a mechanical device that acts as an artificial kidney by removing waste and excess fluid from the blood. It contains semi-permeable membranes made of thin fibers with microscopic pores that allow small molecules like toxins and water to pass through but keep larger molecules like blood cells and protein inside the blood. Modern dialyzers consist of hollow fiber membranes encased in a rigid cylindrical casing and can filter the equivalent area of 1-2 square meters. Dialyzers come in external, implantable, and wearable forms to provide hemodialysis treatment for kidney failure patients.