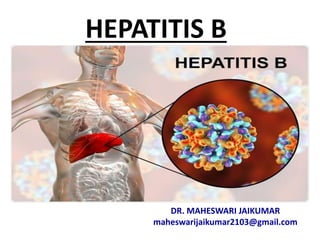
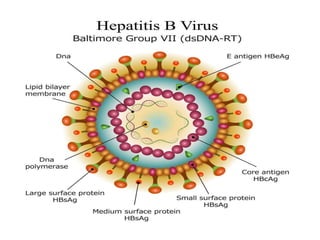
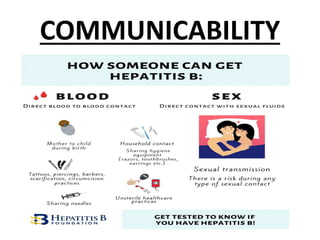
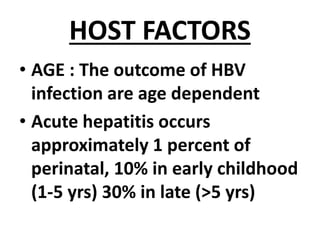
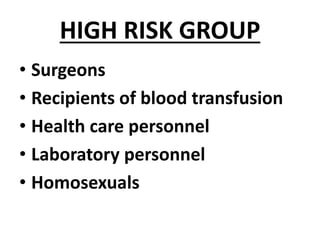
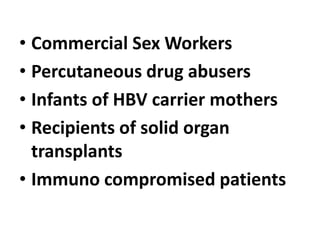
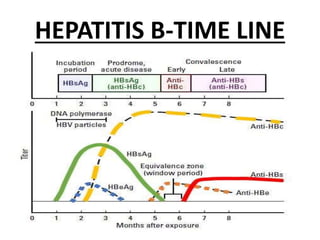
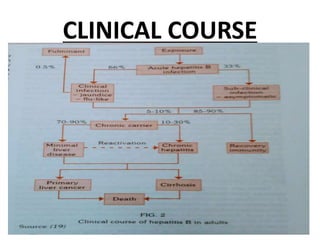
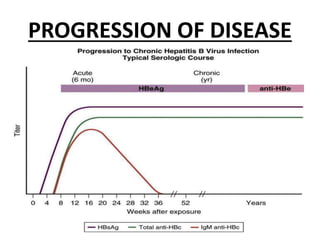
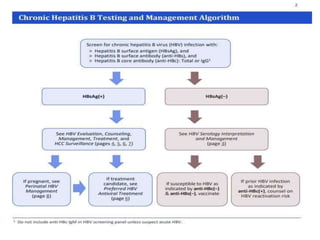
Hepatitis B is caused by the hepatitis B virus (HBV) and causes liver infection and inflammation. It is transmitted through contact with infected blood or bodily fluids. HBV can cause both acute and chronic infection. Chronic infection may lead to serious complications like cirrhosis and liver cancer. Hepatitis B is preventable through vaccination, which induces protective antibody levels in over 95% of people vaccinated.