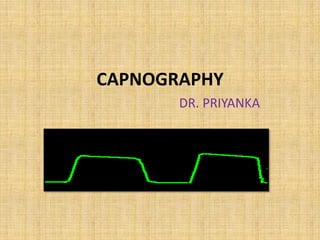
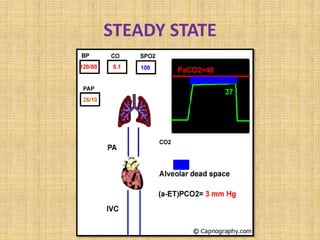
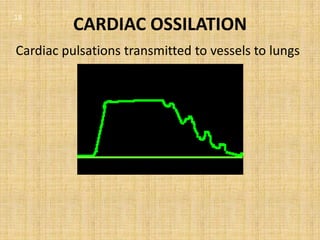
Capnography is the measurement of carbon dioxide in respiratory gases and is an integral part of anesthesia monitoring. It was developed in the 1940s and standards now recommend its use for basic monitoring during anesthesia. Capnography can be used to monitor respiration rate, verify endotracheal tube placement, detect circuit disconnections or leaks, and help diagnose various respiratory and circulatory conditions based on the shape of the capnography waveform. It provides important real-time information about a patient's ventilation and metabolism.