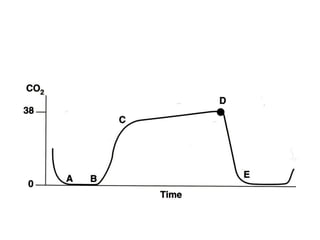
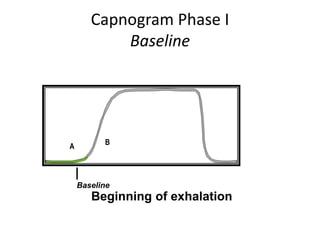
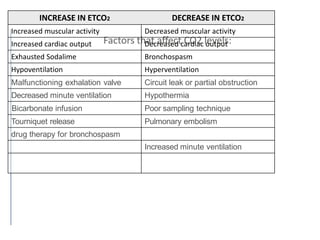
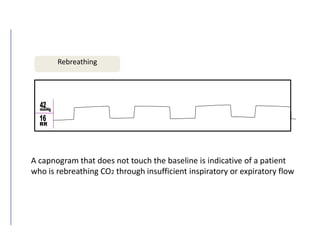
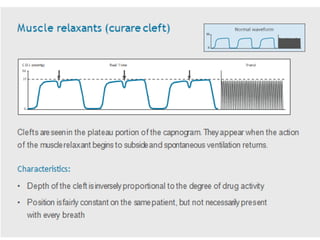
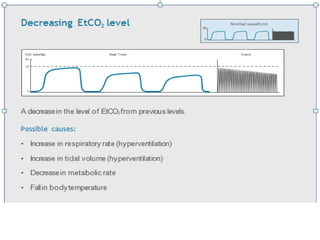
Capnography is used to continuously monitor carbon dioxide levels in exhaled breath. It provides information about ventilation by measuring end-tidal carbon dioxide (EtCO2). The capnogram displays breath-by-breath CO2 levels and has four phases - phases I and IV show no CO2 as air is in the dead space, phase II is the ascending slope as alveolar gas mixes with dead space air, and phase III is the alveolar plateau that shows uniform CO2 levels in exhaled breath and is used to measure EtCO2. Abnormal capnogram waveforms can indicate issues like bronchospasm, esophageal intubation, or rebreathing. Capnography is a useful monitoring



![Capnography
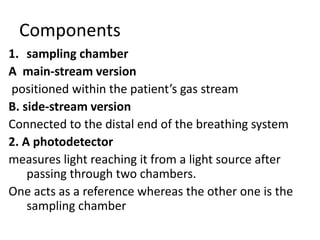
Continuous measurement of patient’s inhaled and exhaled
[CO2]
Waveform display more informative than the value
Useful for evaluation of
– Esophageal intubation
– Disconnect in breathing circuit
– Rebreathing of CO2
– Cardiac arrest
– Malignant Hyperthermia / Thyroid storm
– Hypotension
– PE
ETCO2 underestimates PaCO2 due to deadspace ventilation](https://image.slidesharecdn.com/capnography-191202084615/85/Capnography-6-320.jpg)