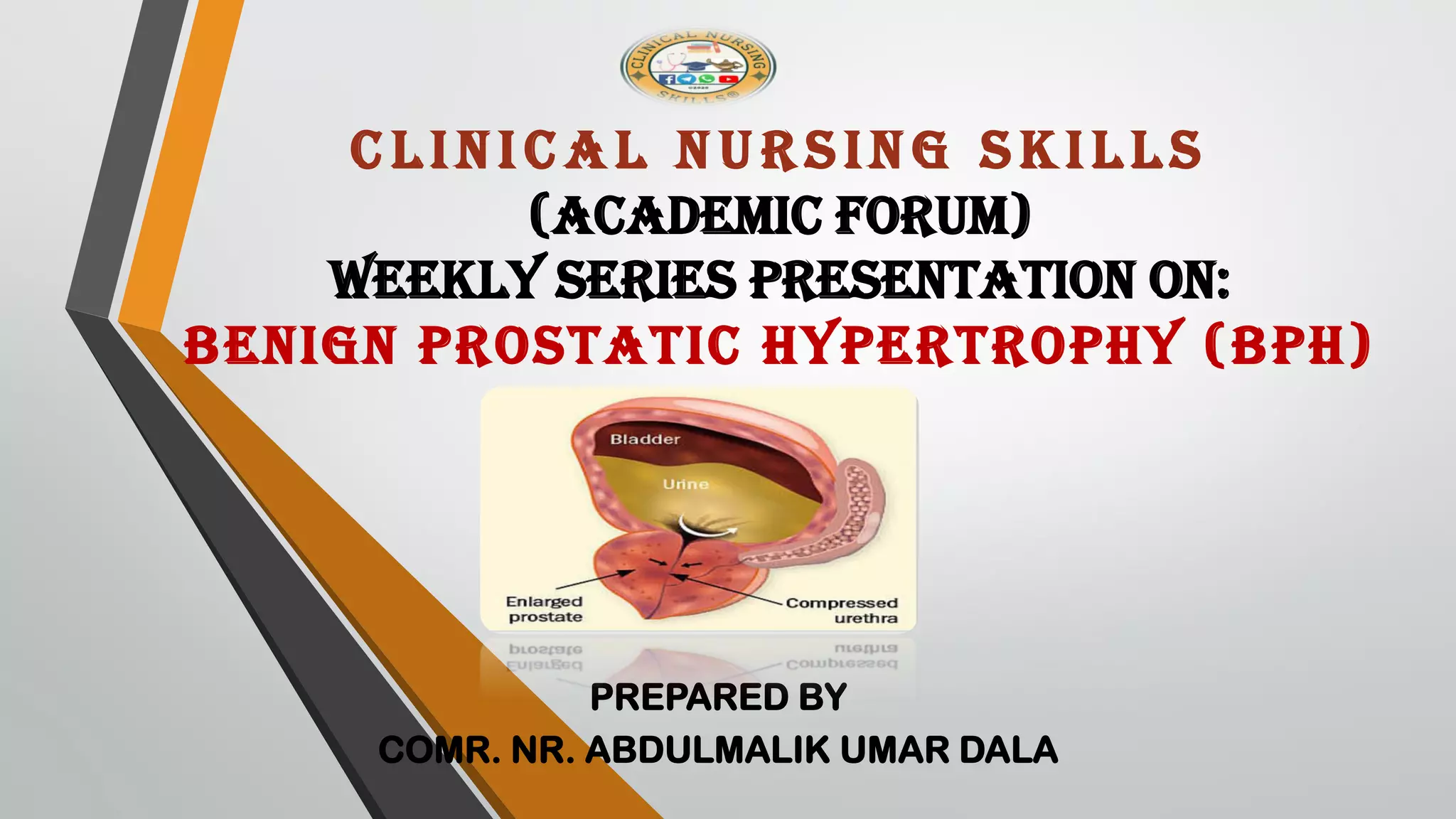
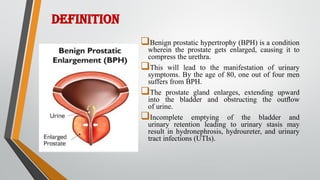
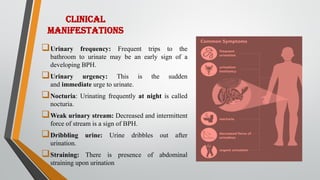
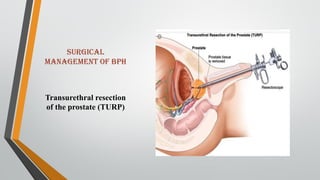
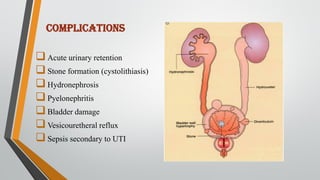
This document provides an overview of benign prostatic hypertrophy (BPH). It defines BPH as a non-cancerous enlargement of the prostate gland that occurs in aging men. Risk factors include elevated estrogen levels, smoking, a sedentary lifestyle, and a high-fat Western diet. Symptoms include frequent and urgent urination, weak urine stream, and incomplete emptying of the bladder. Diagnosis involves digital rectal exam, urinalysis, and prostate-specific antigen testing. Treatment options include medications to relax the prostate like alpha-blockers, surgery to remove part of the prostate, and minimally invasive procedures using heat or radiofrequency energy. Nursing care focuses on relieving discomfort, maintaining fluid balance