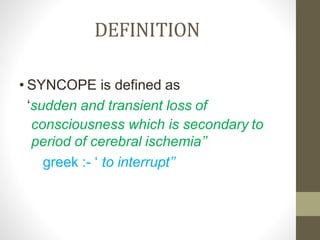
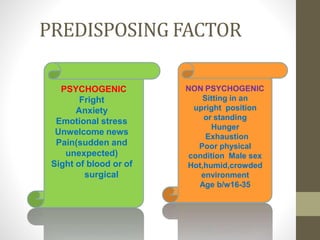
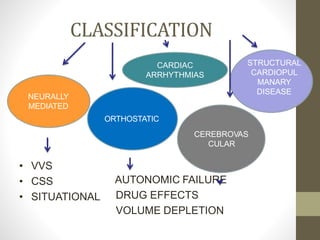
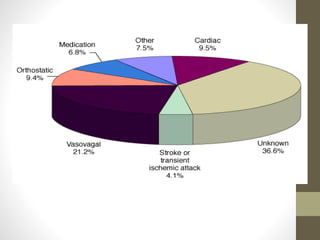
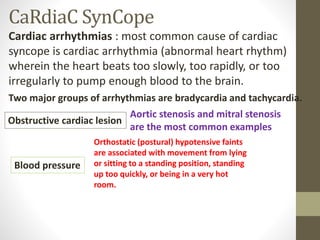
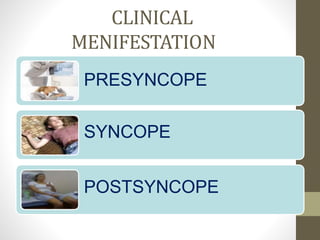
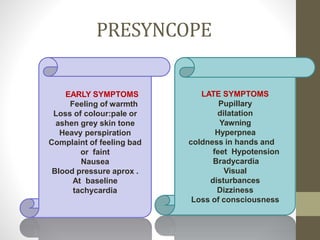
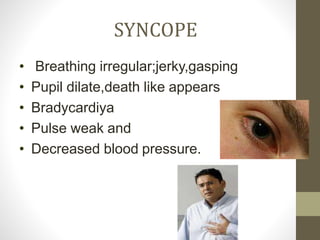
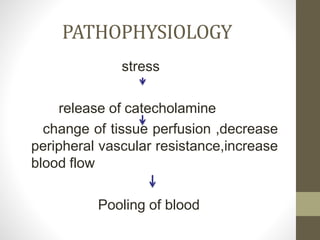
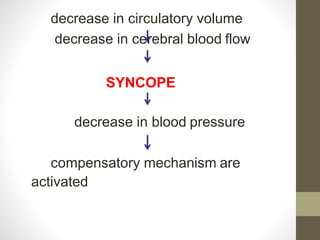
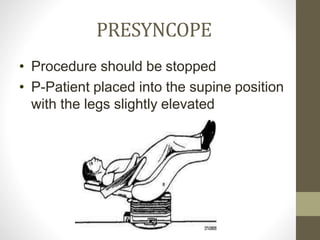
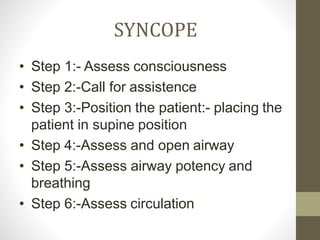
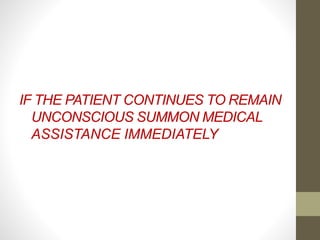
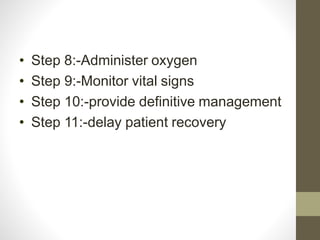
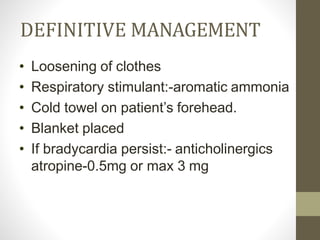
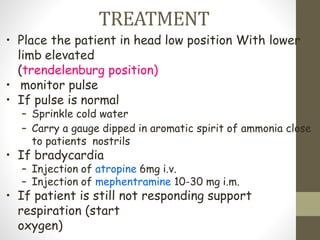
Syncope, or fainting, is defined as a transient loss of consciousness caused by a brief period of low blood flow to the brain. It has many potential causes including vasovagal, cardiac, and neurological factors. Common triggers for vasovagal syncope include pain, emotional stress, and standing for long periods. Symptoms progress from presyncope like dizziness to loss of consciousness during a syncopal episode. Treatment depends on the identified cause but generally involves lying the patient flat and monitoring their vital signs until recovery. Further cardiac workup may be needed to rule out serious arrhythmias or structural issues in some cases.