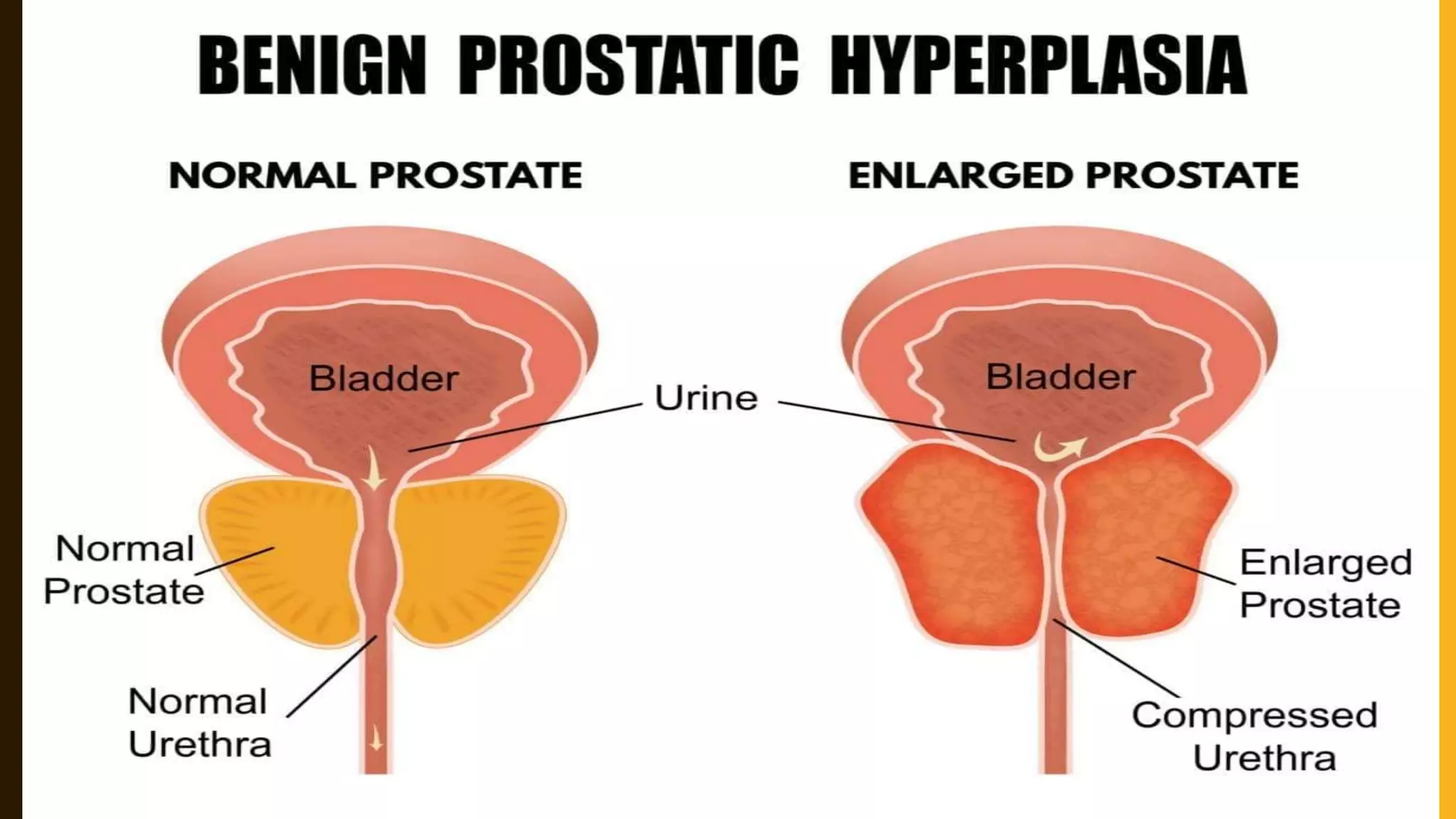
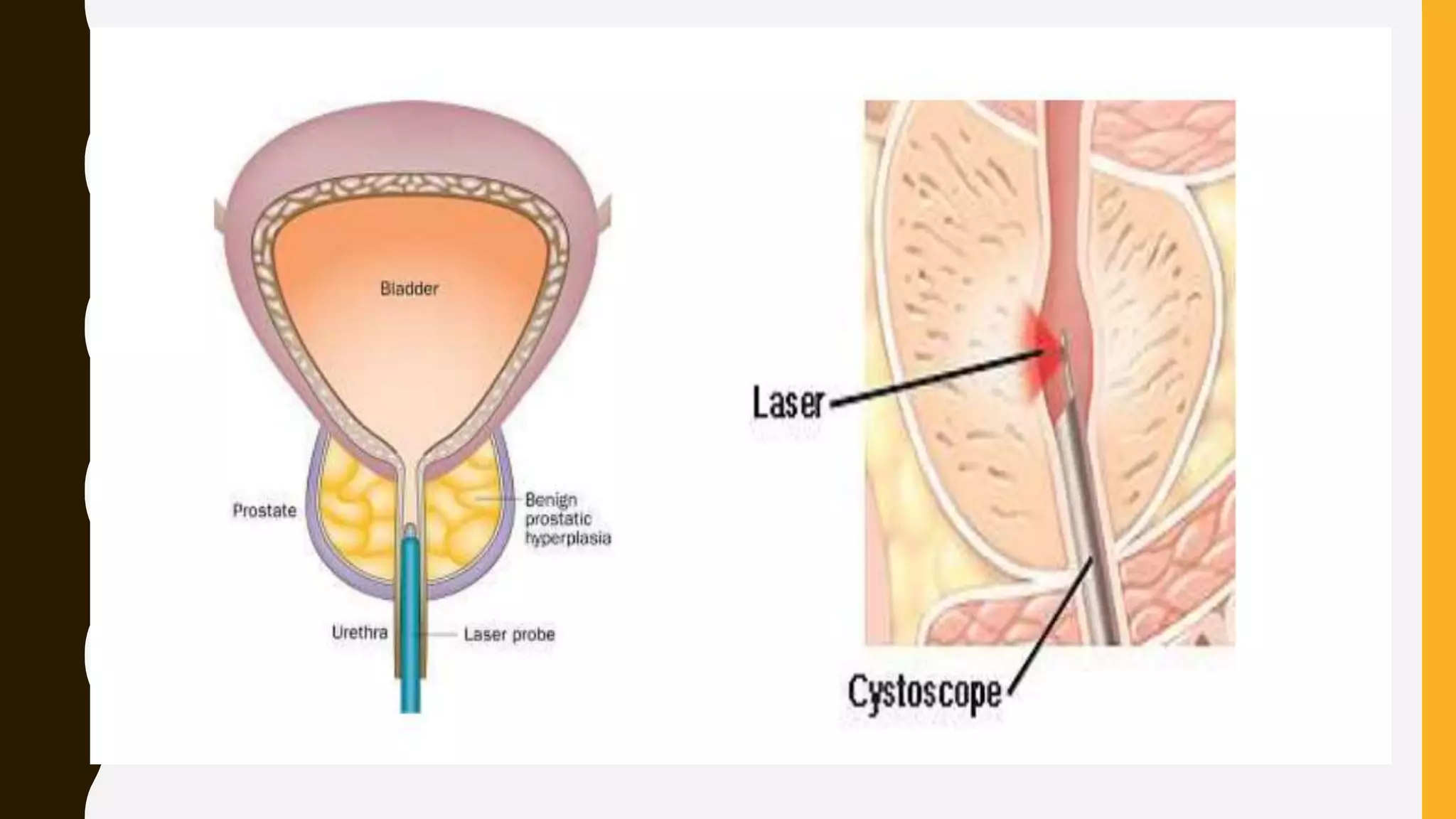
Benign prostatic enlargement is a common condition in aging men that causes the prostate gland to enlarge and squeeze the urethra, slowing urine flow. It has no known cause but risk increases with age. Symptoms include frequent and urgent urination. Diagnosis involves medical history, physical exam, and tests like PSA. Treatment options include medications to shrink the prostate, surgery to remove parts of it, or procedures using heat therapy. Nursing care focuses on monitoring urine output, preventing infection, and teaching patients self-care.