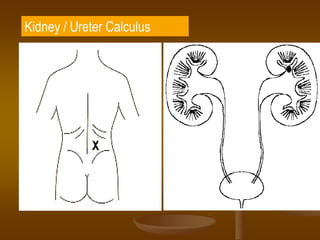
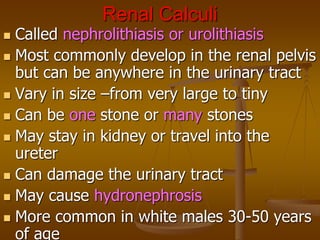
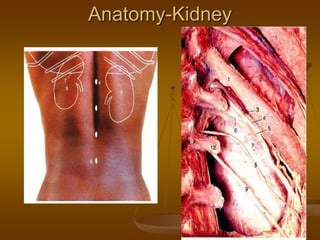
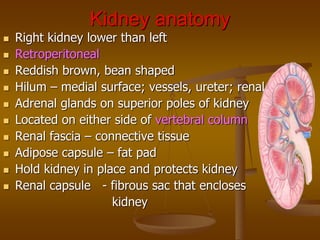
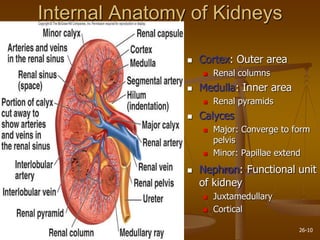
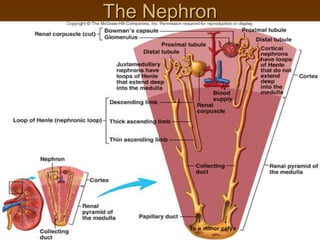
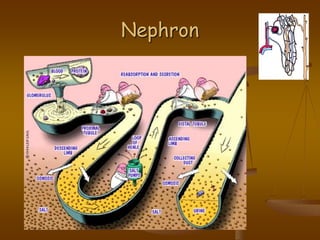
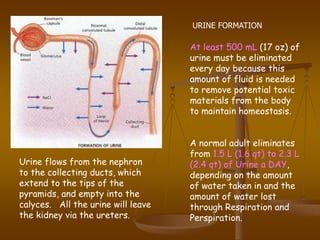
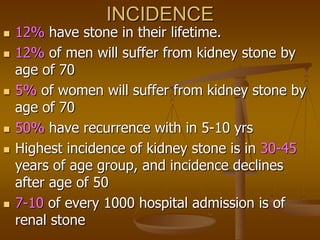
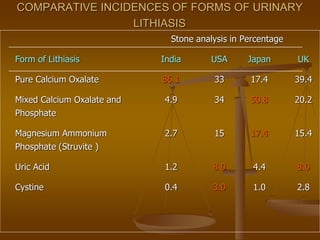
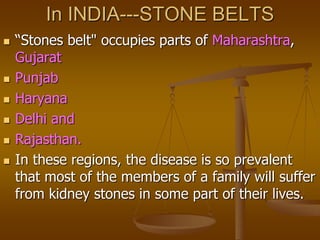
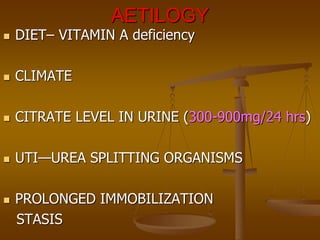
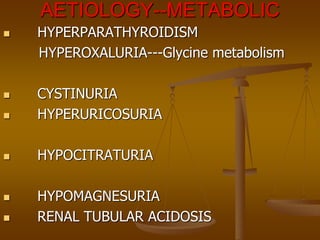
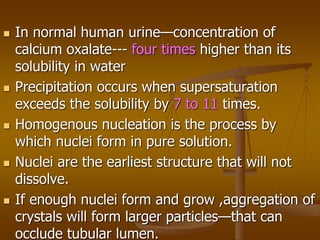
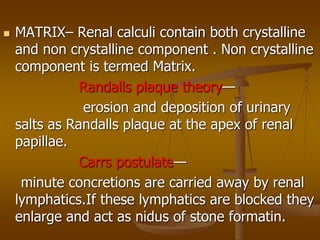
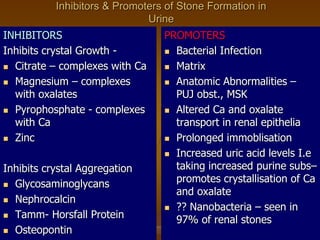
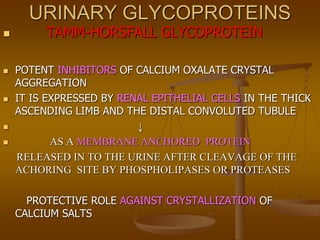
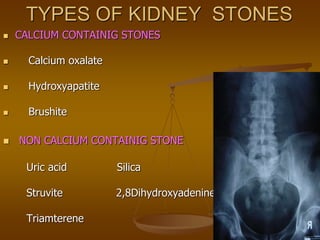
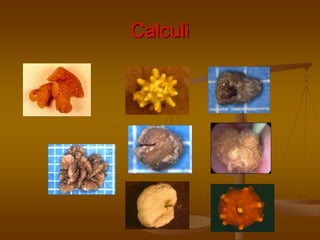
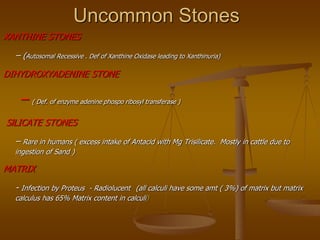
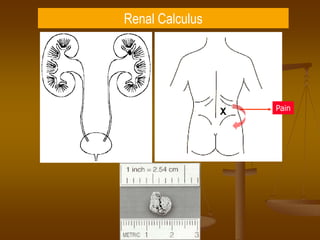
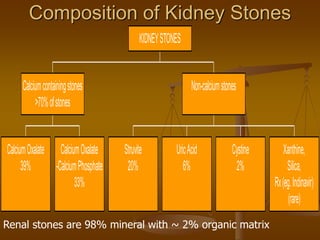
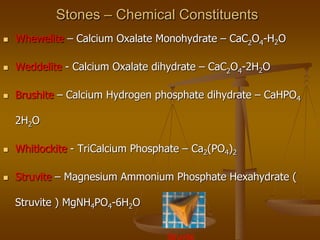
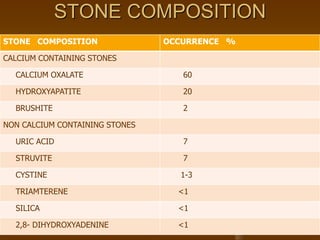
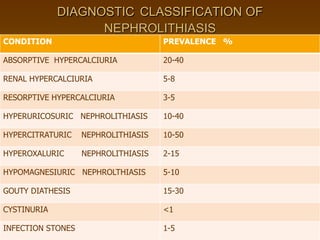
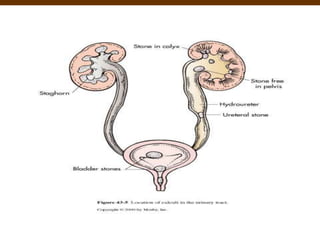
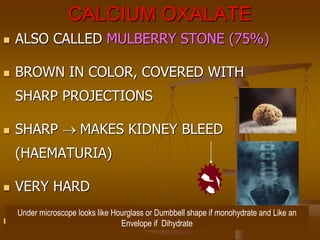
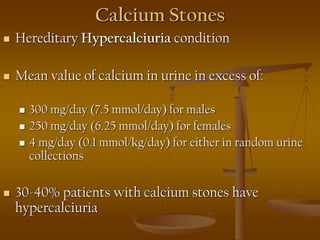
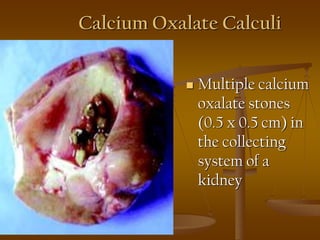
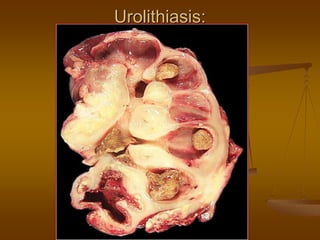
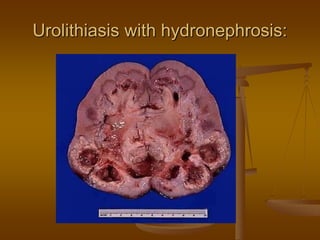
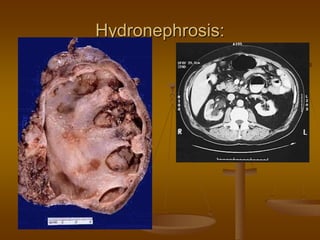
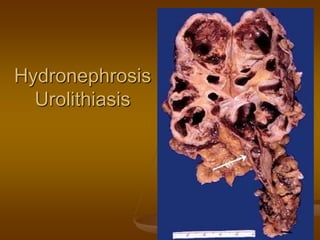
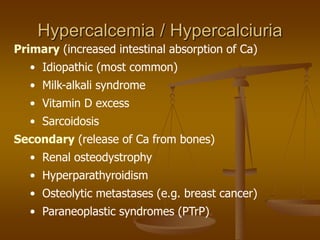
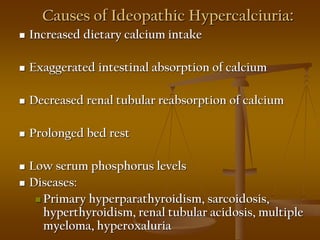
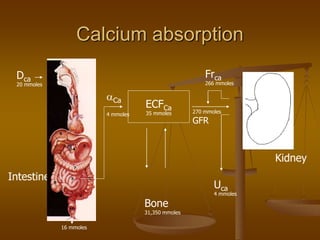
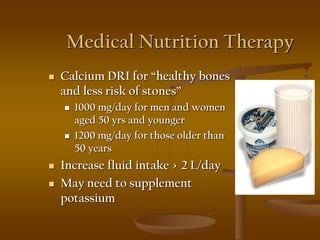
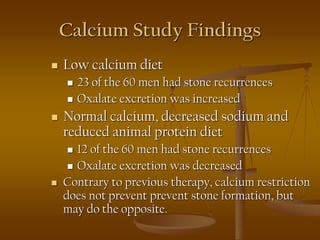
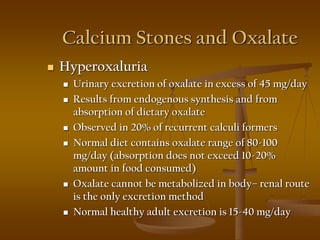
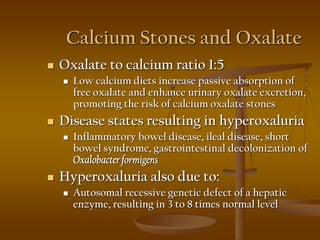
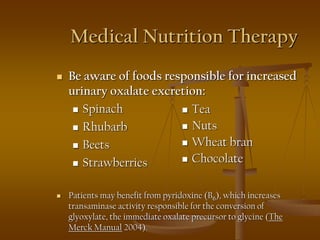
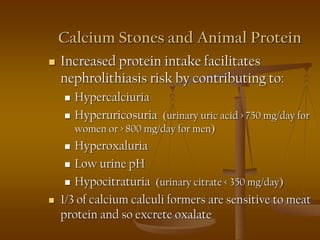
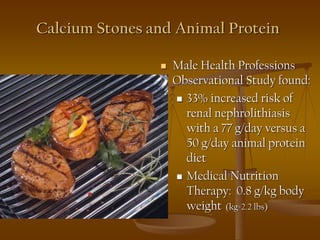
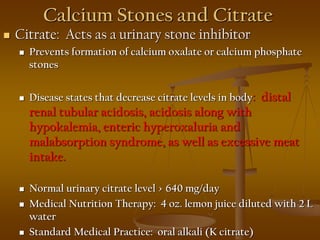
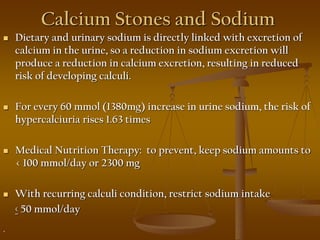
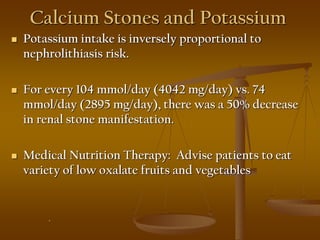
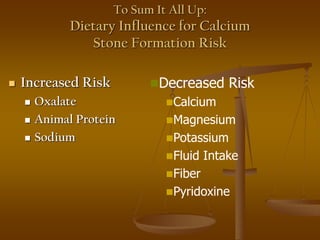
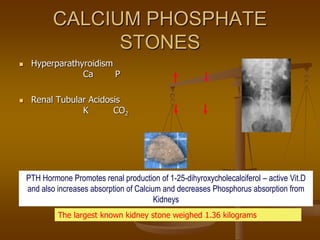
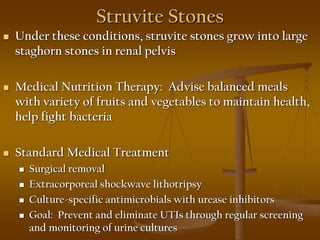
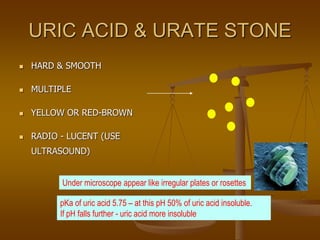
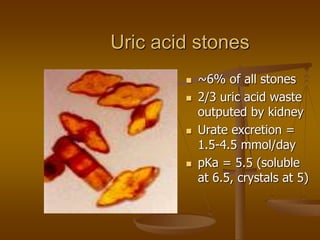
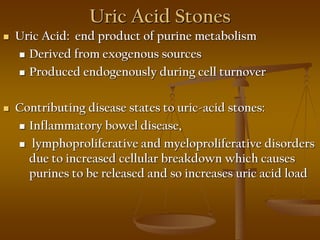
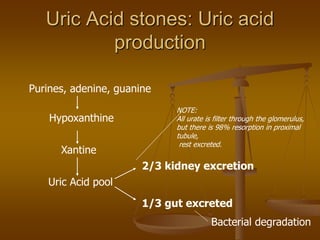
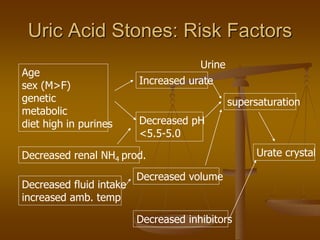
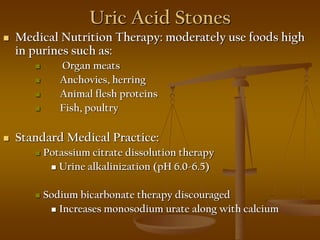
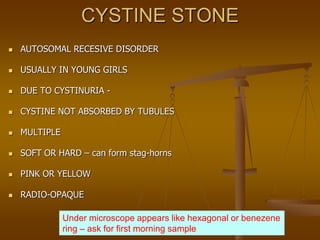
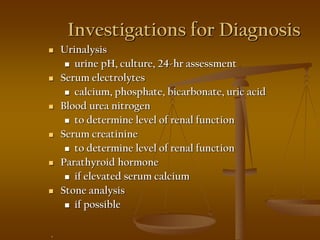
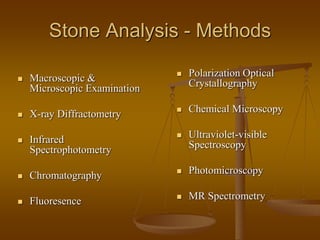
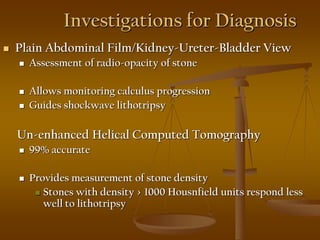
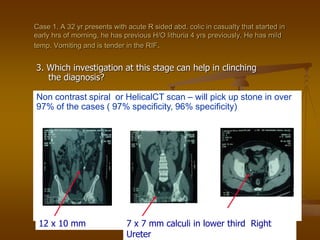
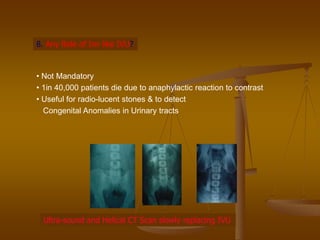
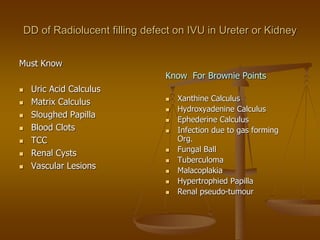
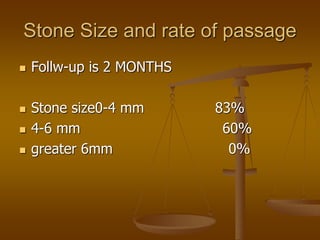
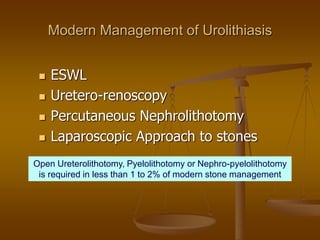
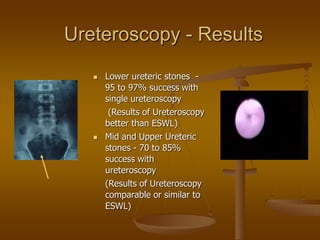
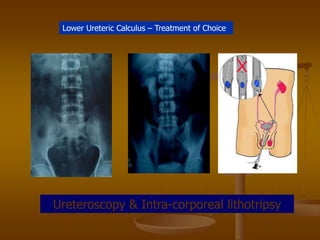
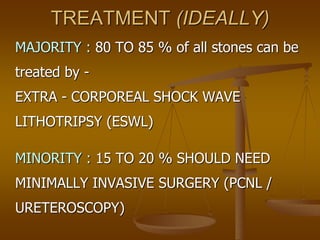
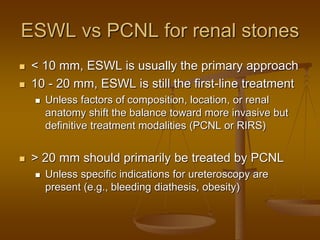
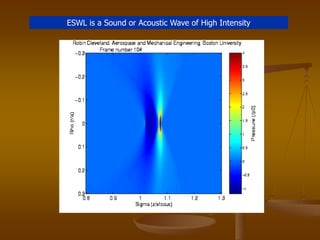
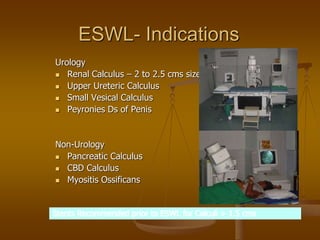
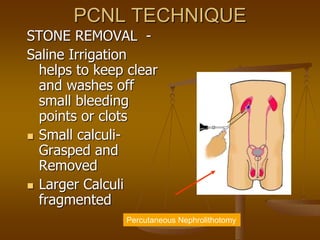
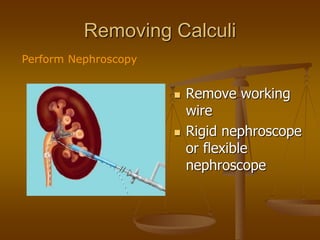
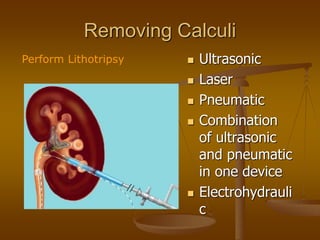
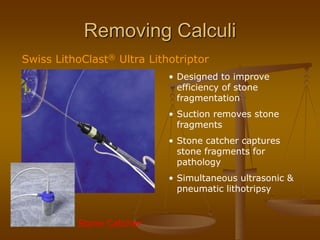
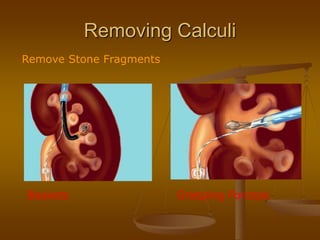
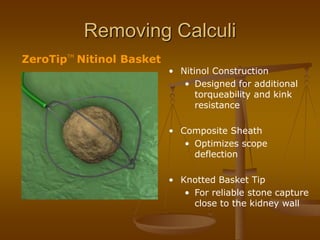
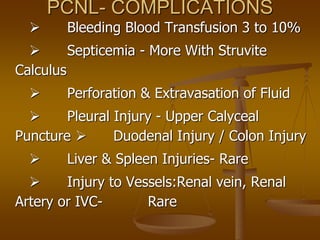
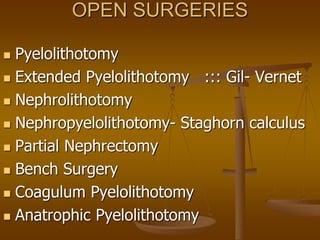
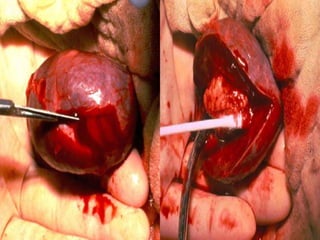
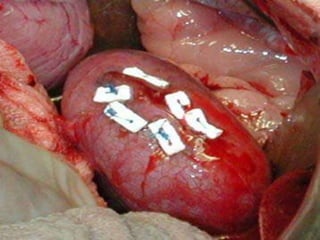
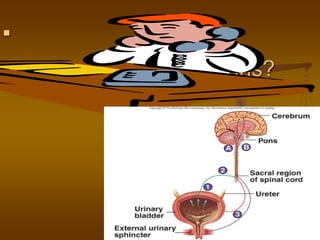
This document summarizes a presentation on renal stone disease. It discusses the anatomy of the kidneys and nephrons, stages of stone formation, types of stones including calcium oxalate and uric acid stones, investigations for stones, and medical and surgical management options. It notes that calcium oxalate is the most common stone type, occurring in over 75% of cases. Dietary and metabolic factors that can promote stone formation like hypercalciuria and hyperoxaluria are also outlined.