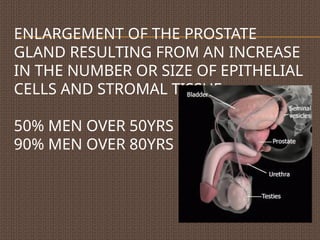
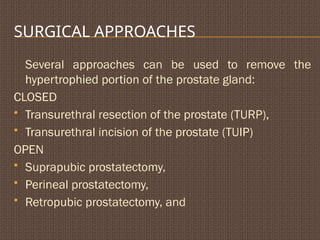
Benign prostate hypertrophy (BPH) involves enlargement of the prostate gland affecting over 50% of men over 50 years. The condition is influenced by age, hormonal factors, and lifestyle, leading to urinary symptoms and potential complications like urinary retention and infections. Management options include lifestyle changes, medications, and various surgical procedures tailored to the severity of the condition.
![ETIOLOGY
Ageing
Excessive accumulation of prostatic androgen
[dihydroxytestosterone]
Stimulation by estrogen
Local growth hormone action](https://image.slidesharecdn.com/benignprostatehypertrophy-240831164604-2d36027f/85/benign-prostate-hypertrophy-pptxlllllll-m-3-320.jpg)
![RISK FACTORS
Family history
Environment
Diet [saturated fatty acids]
Reduced exercise
Alcohol consumption](https://image.slidesharecdn.com/benignprostatehypertrophy-240831164604-2d36027f/85/benign-prostate-hypertrophy-pptxlllllll-m-4-320.jpg)
![DIAGNOSTICS
History & PE
Digital Rectal examinaton
Urinalysis
Urine c/s
PSA [Prostate specific antigen]
Transrectal ultrasound
Uroflowmetry
Measure Postvoidal residual urine
Cystourethroscopy](https://image.slidesharecdn.com/benignprostatehypertrophy-240831164604-2d36027f/85/benign-prostate-hypertrophy-pptxlllllll-m-7-320.jpg)


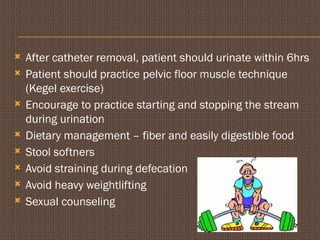
![POSTOPERATIVE
main complications- hemorrhage, bladder spasms,
urinary incontinence, infections
Bladder irrigations with normal saline [pink, no clots]
Monitor inflow & outflow of irrigant
Catheter care
avoid activities that increase the abdominal pressure
To relieve bladder spasms- opium suppositories,
antispasmodics with relaxation techniques.](https://image.slidesharecdn.com/benignprostatehypertrophy-240831164604-2d36027f/85/benign-prostate-hypertrophy-pptxlllllll-m-21-320.jpg)