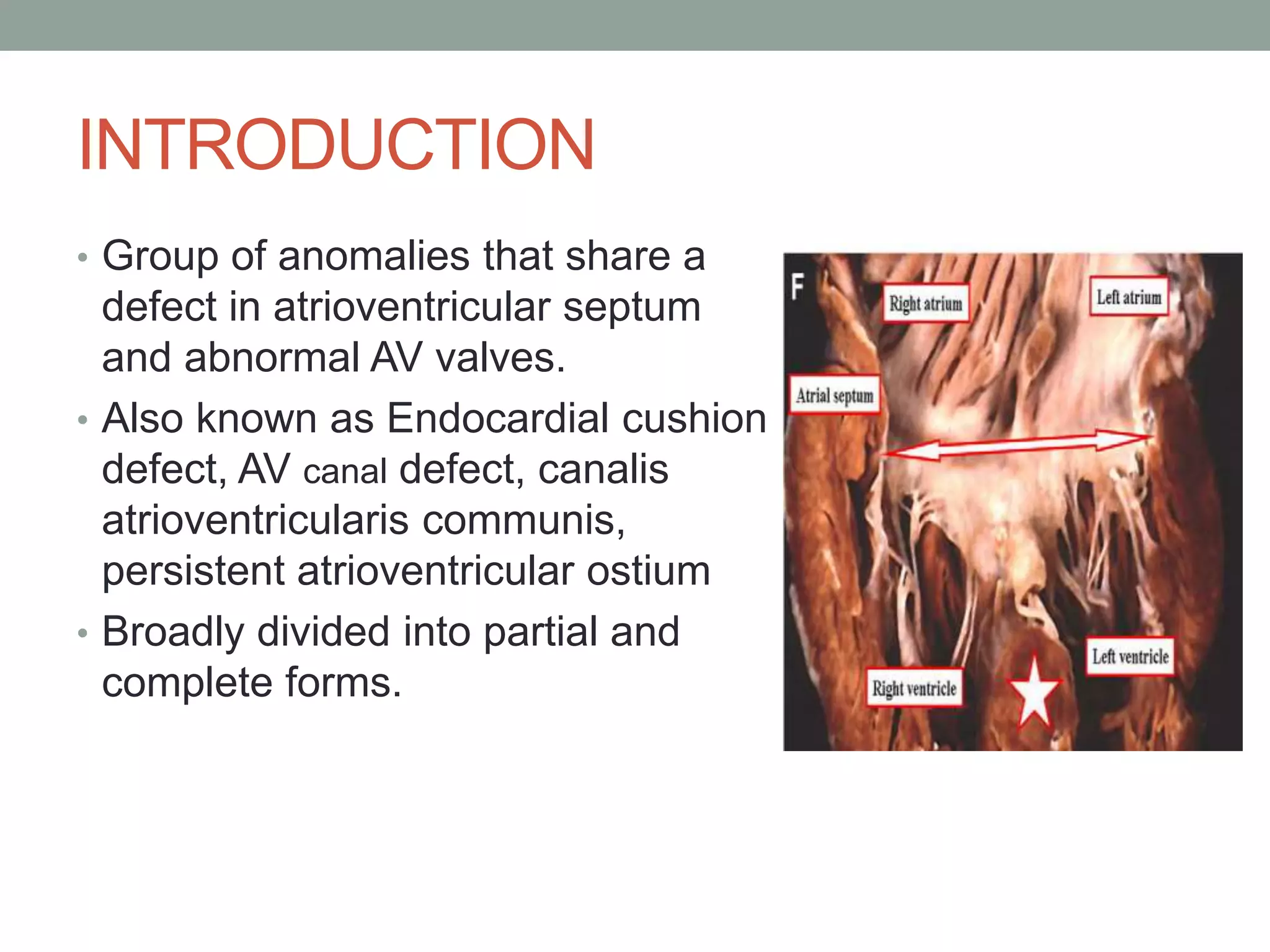
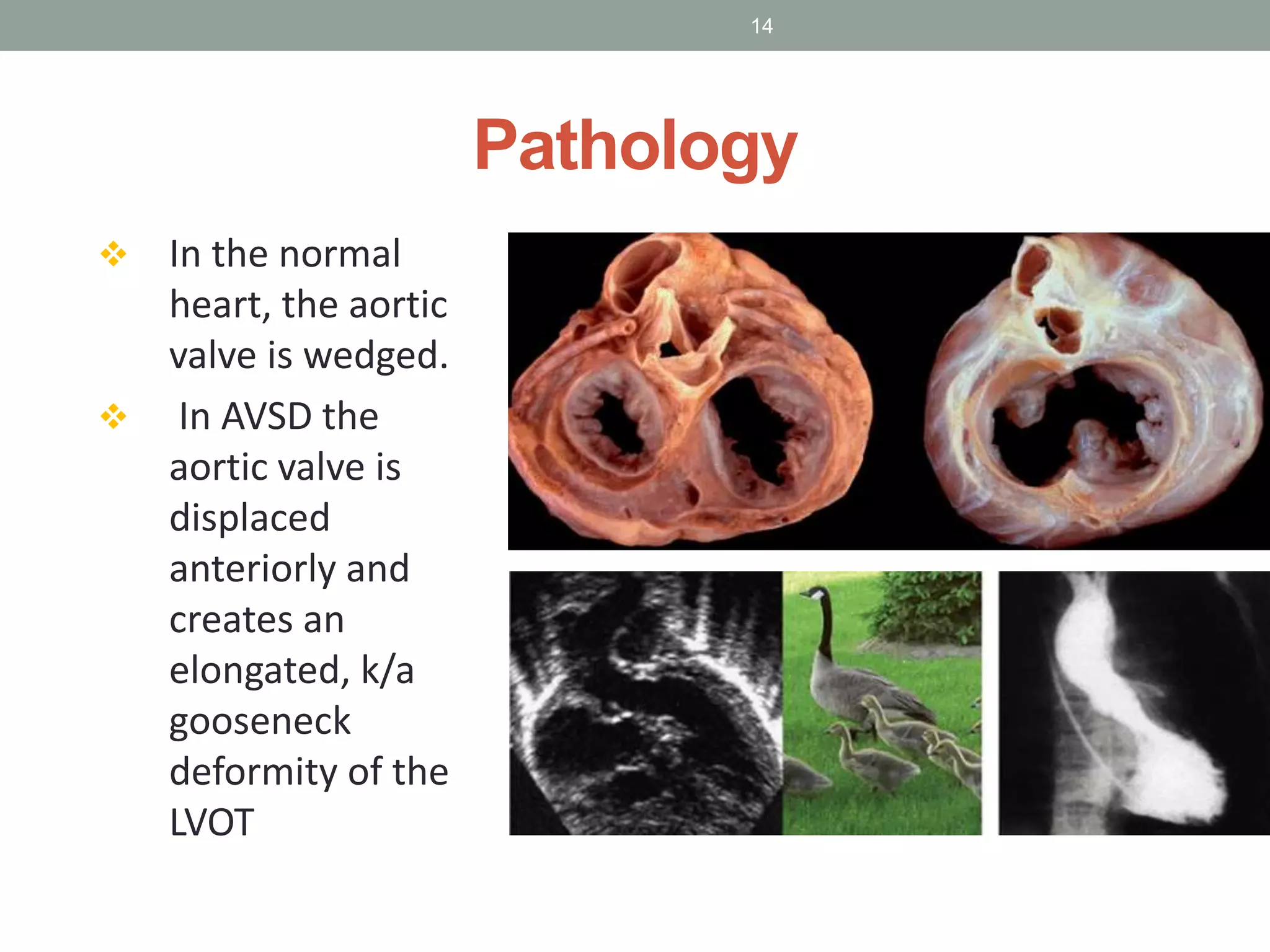
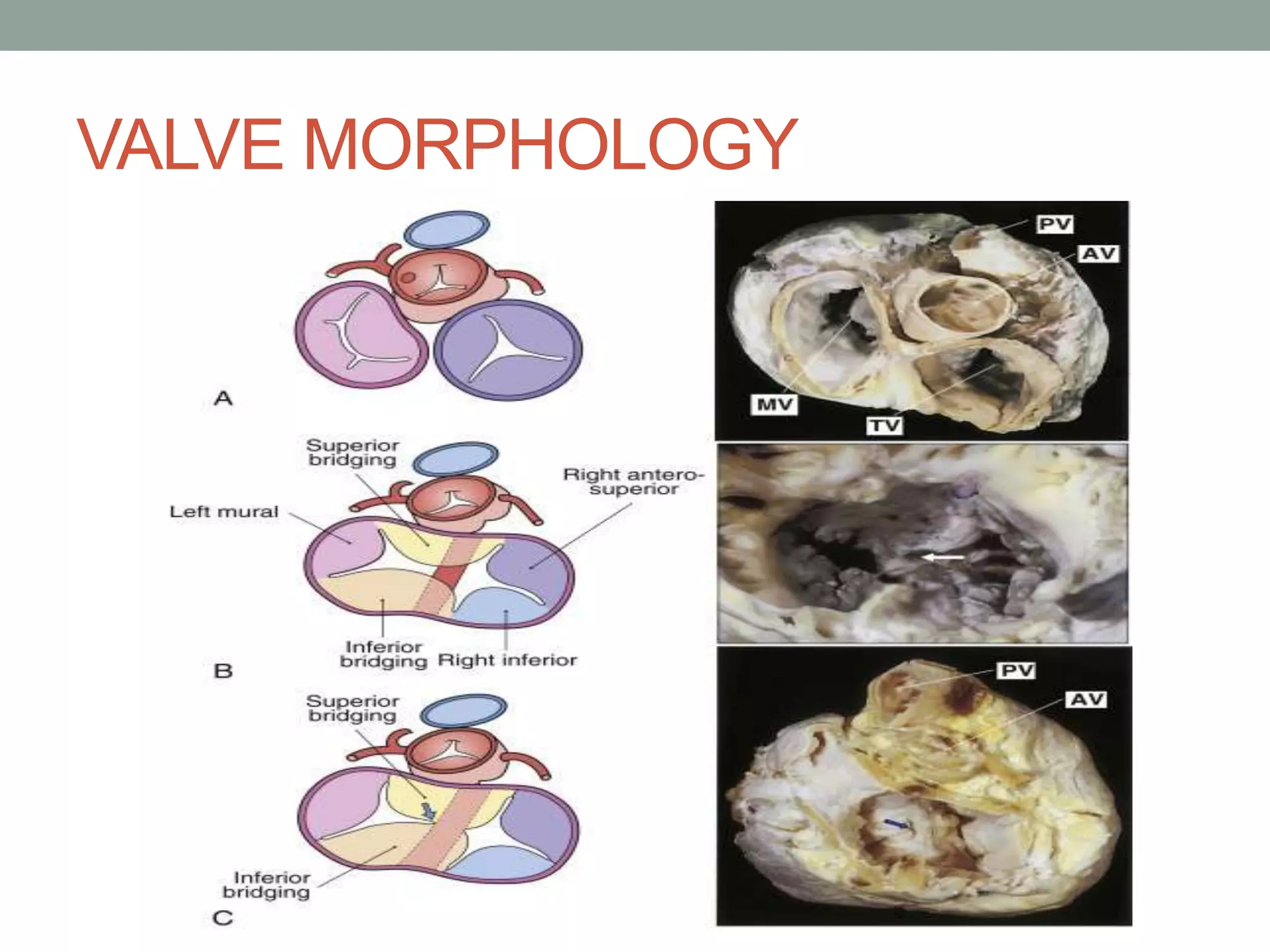
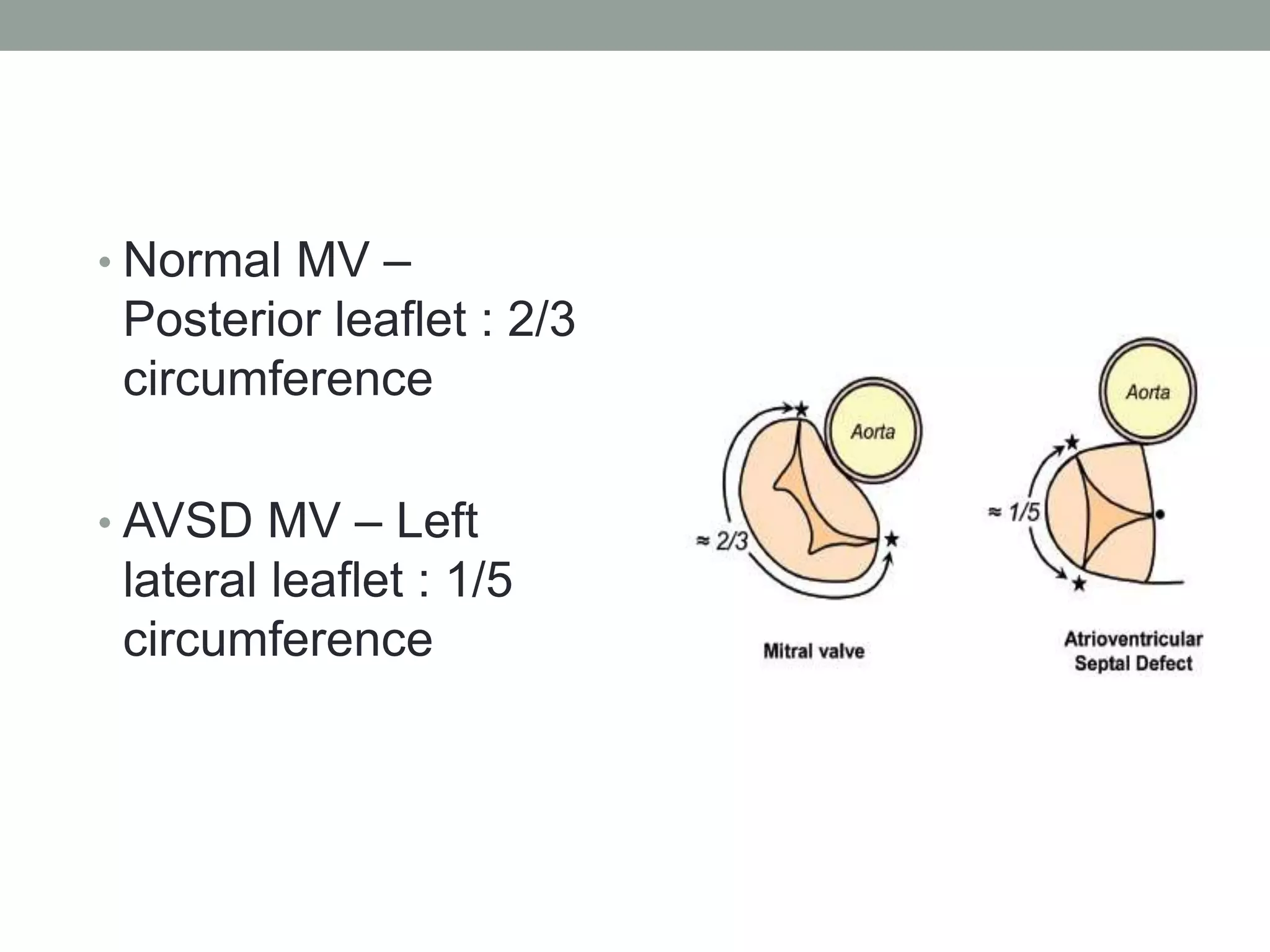
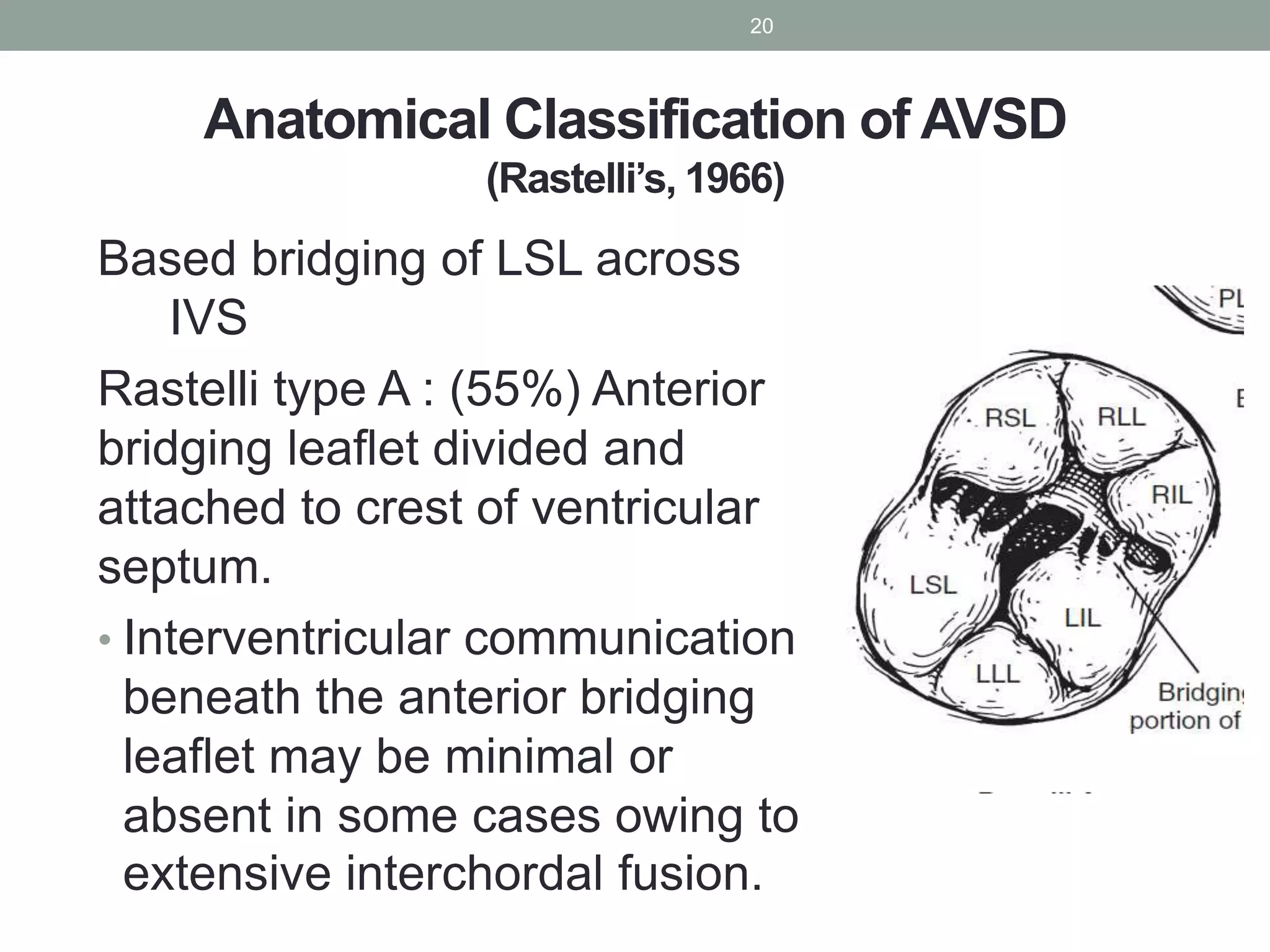
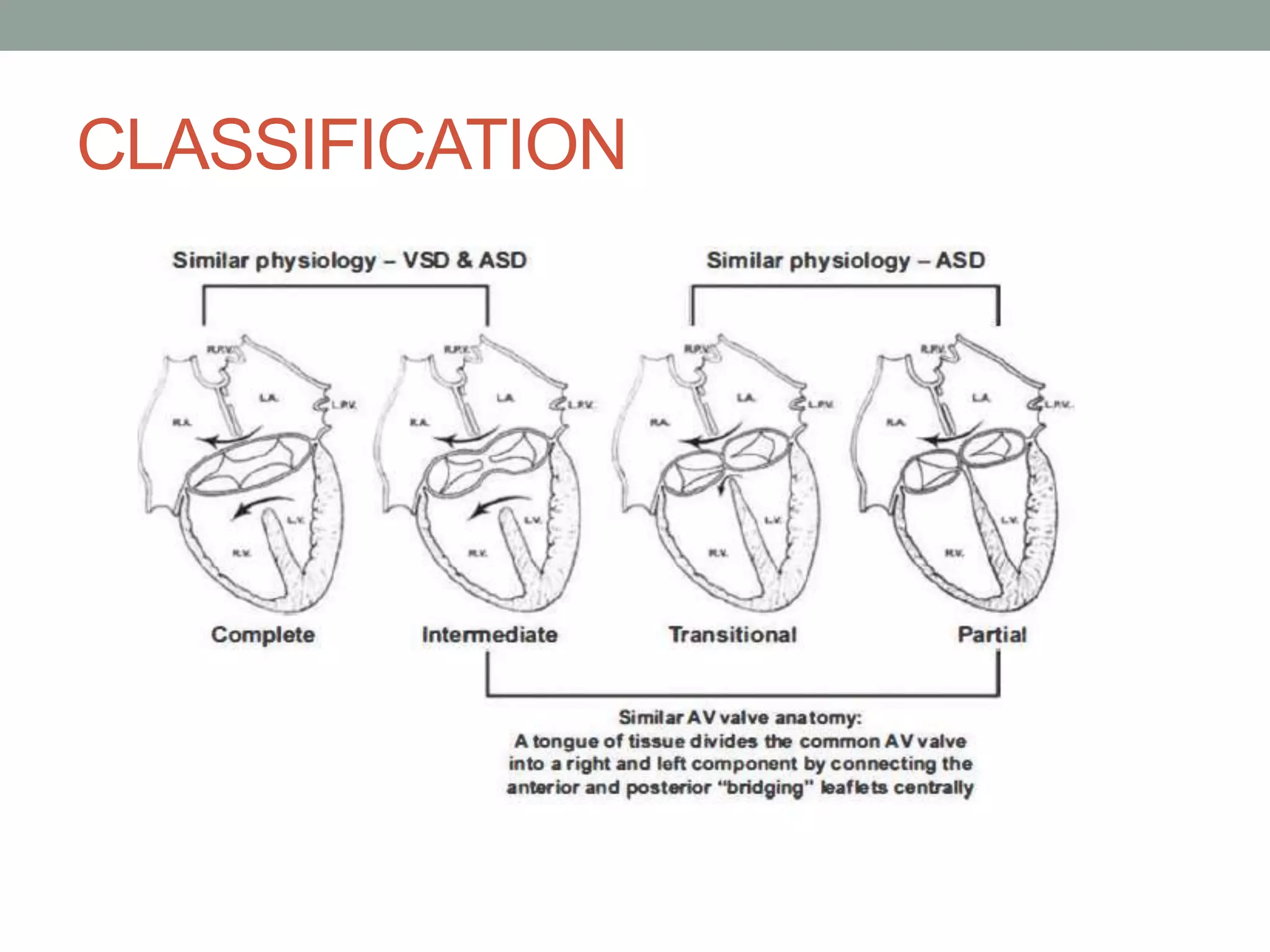
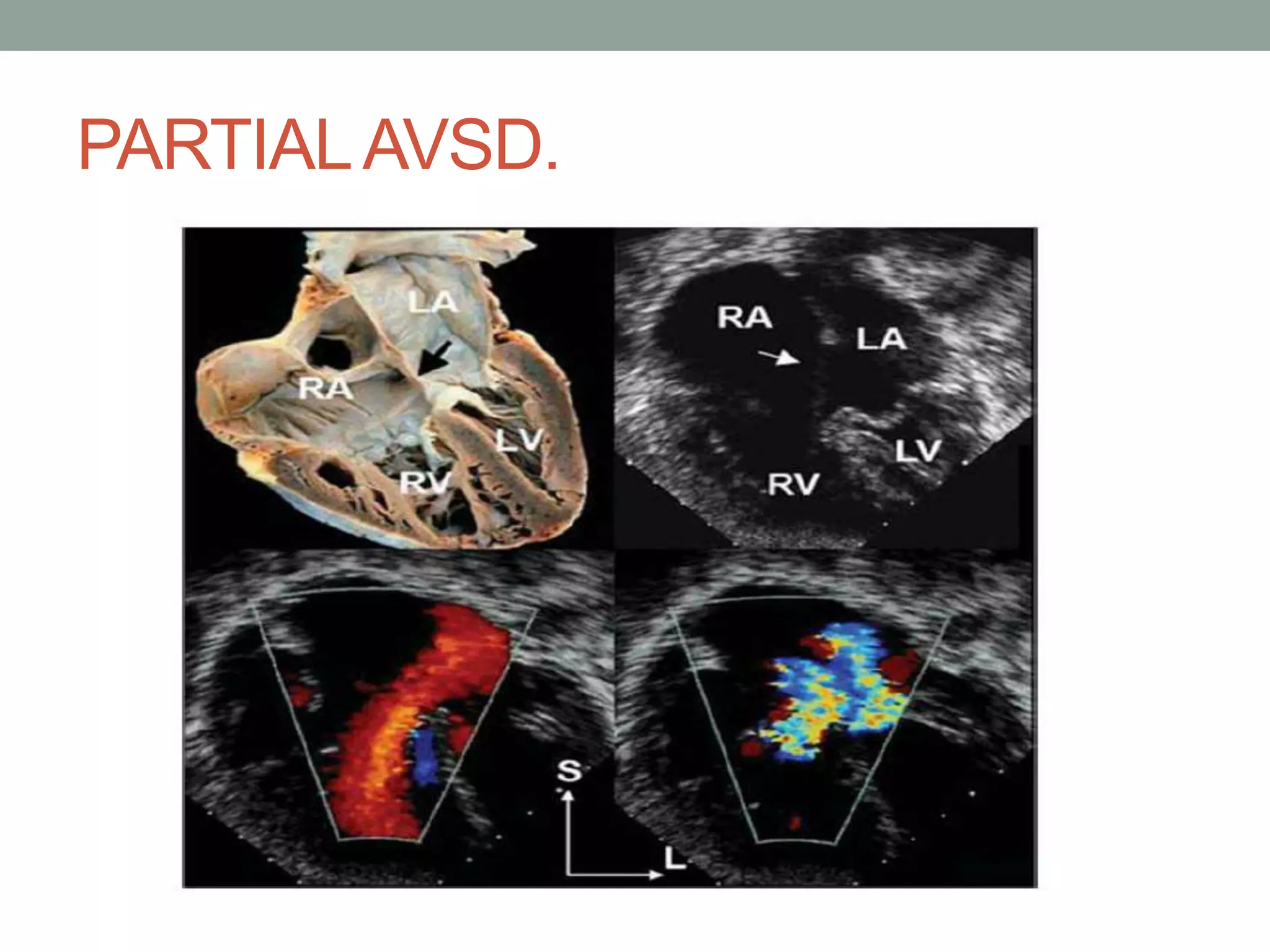
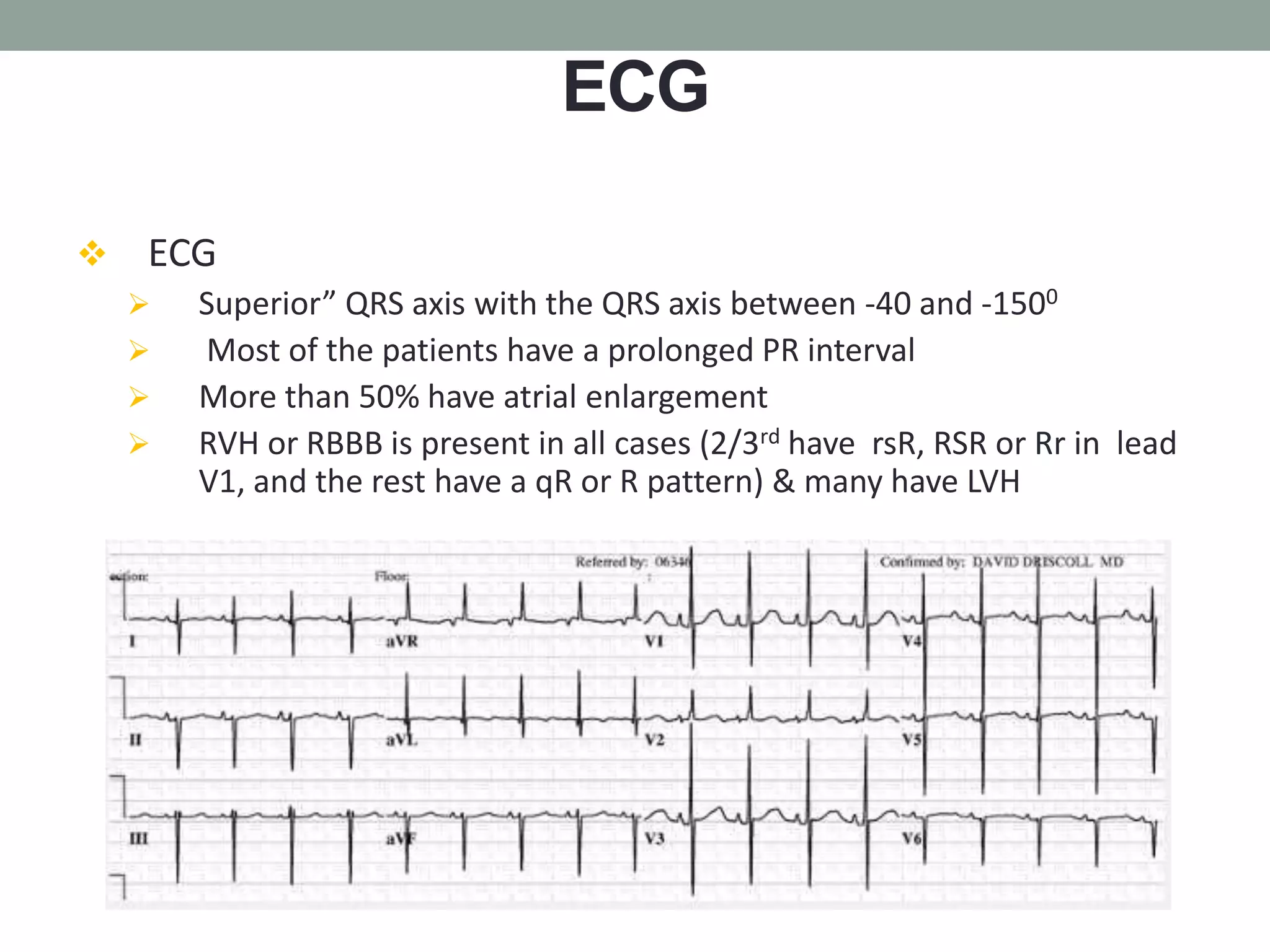
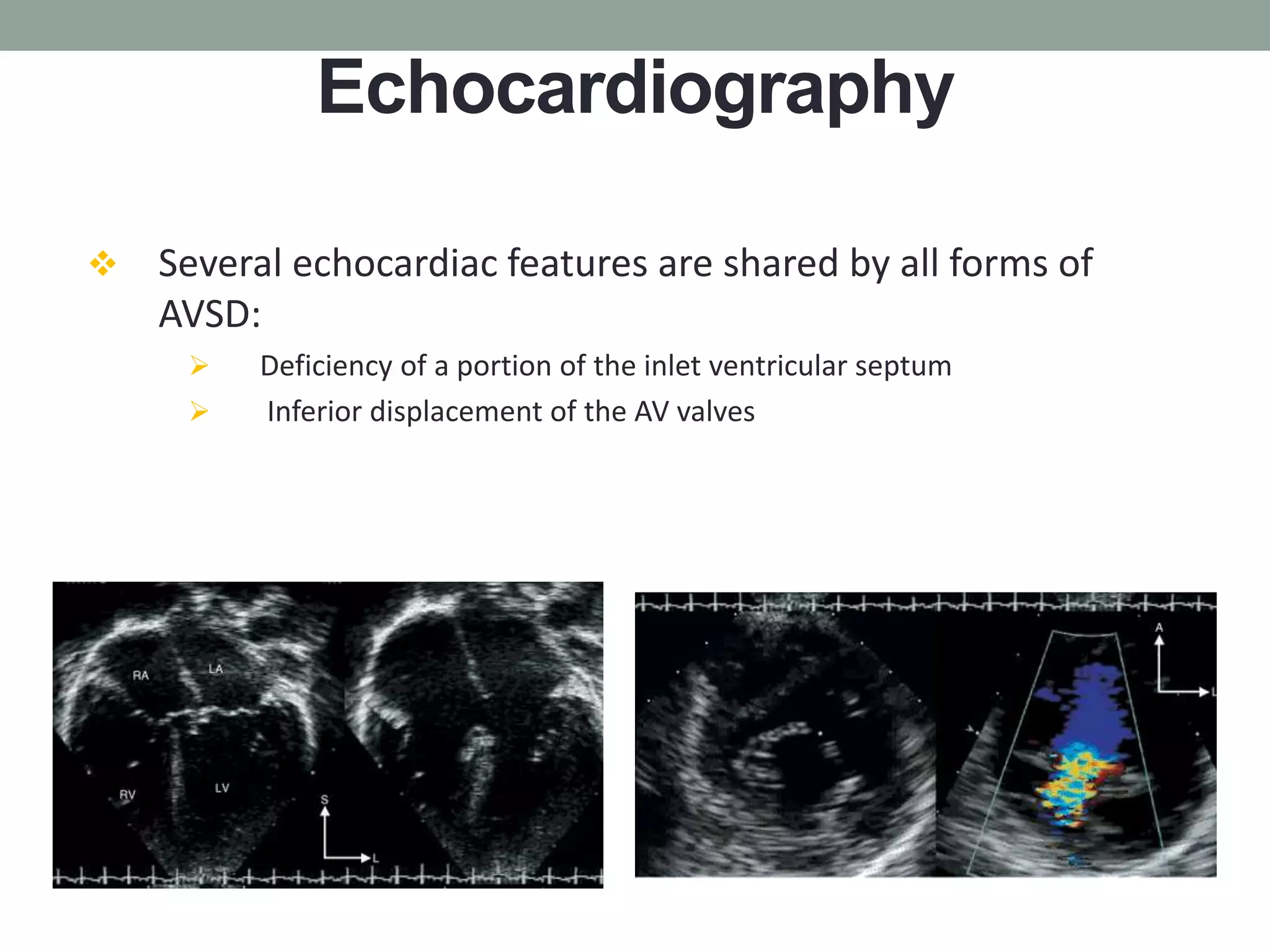
Atrioventricular septal defects (AVSDs) are congenital heart defects involving a defect in the atrioventricular septum and abnormal atrioventricular valves. They are broadly divided into partial and complete forms. Complete AVSD is associated with lack of fusion between the superior and inferior endocardial cushions and requires early surgical repair in infancy to prevent heart failure. Partial AVSD involves an incomplete fusion resulting in a cleft left anterior heart valve, and surgical repair is typically performed later in childhood. Early surgical repair is indicated for complete AVSD and partial AVSD with significant heart valve issues, while stable partial defects may be repaired later in childhood.