1. The document discusses various types of bradycardia and conduction blocks including sinus bradycardia, sick sinus syndrome, different degrees of AV block, bundle branch blocks, and fascicular blocks.
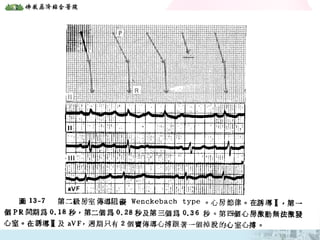
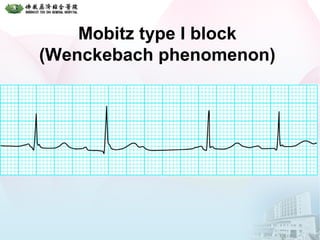
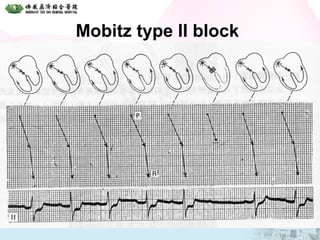
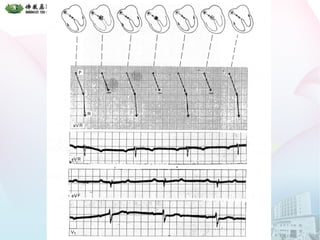
2. It provides details on the characteristics, causes, and electrocardiographic features of each type of block. First degree AV block results in a prolonged PR interval while second degree block causes intermittent failure of conduction.
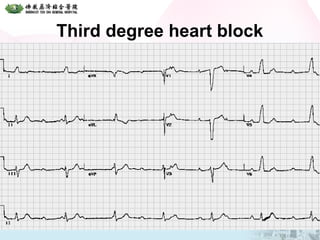
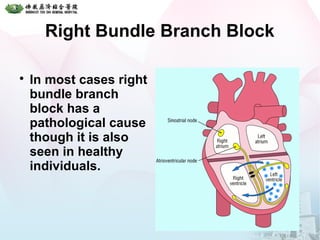
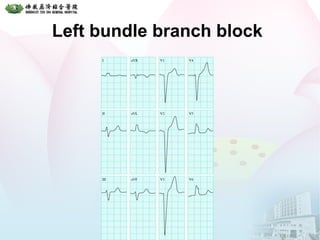
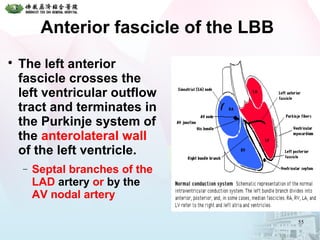
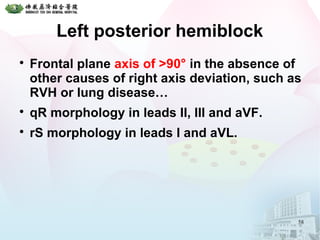
3. Third degree or complete heart block results in independent atrial and ventricular rhythms. Bundle branch blocks involve the right or left bundle branches and fascicular blocks occur in the fascicles of the left bundle branch. Bifascicular and trifascicular blocks involve multiple levels of block