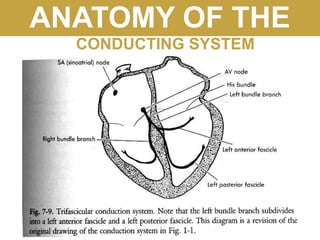
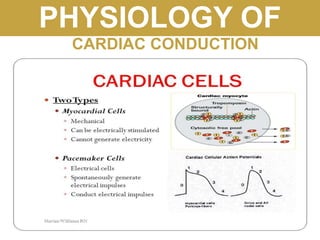
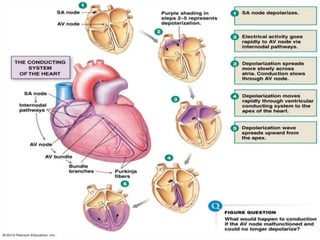
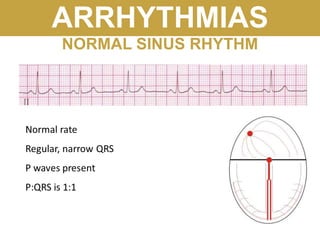
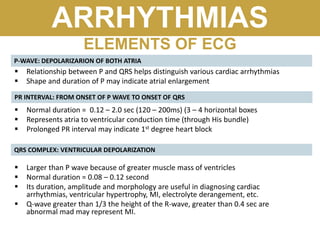
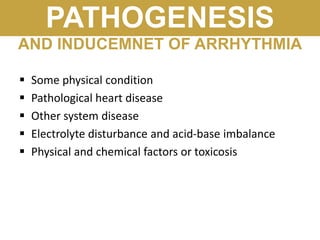
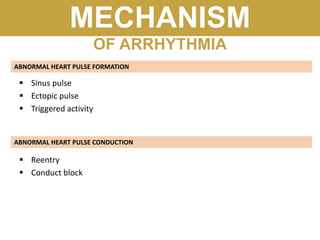
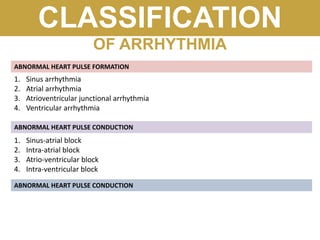
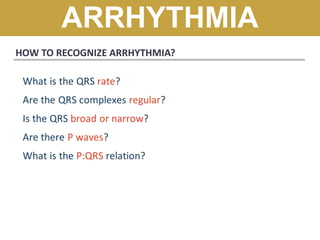
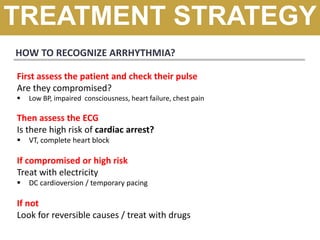
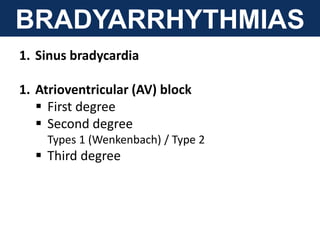
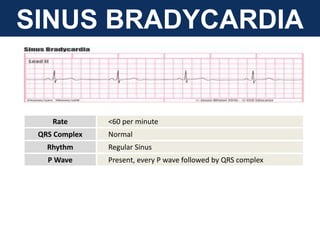
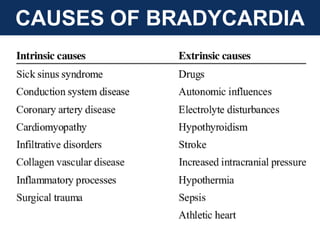
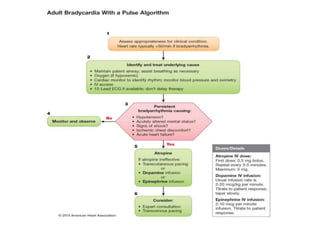
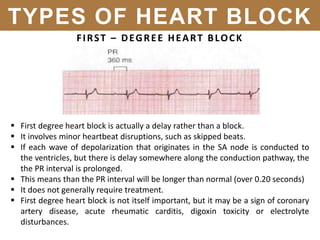
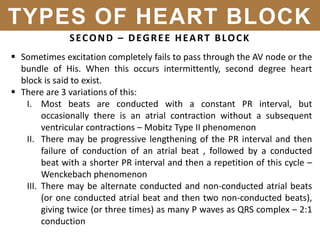
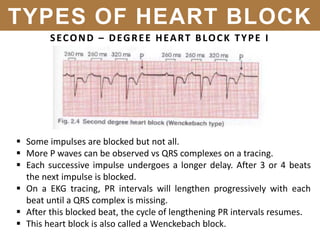
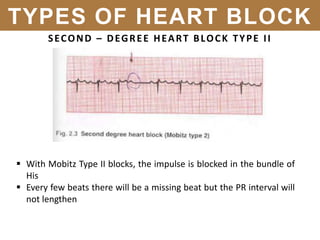
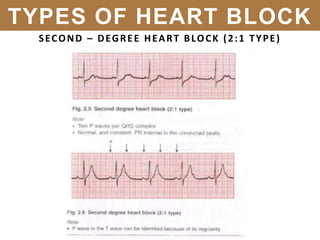
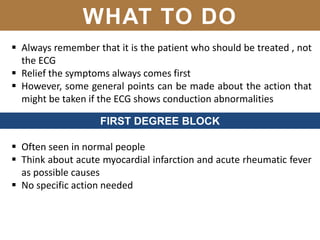
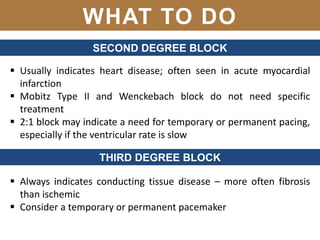
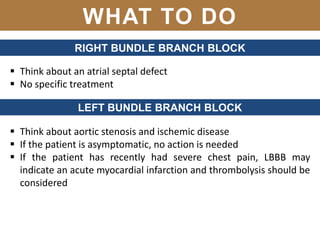
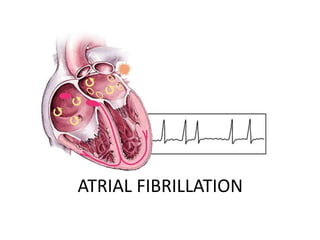
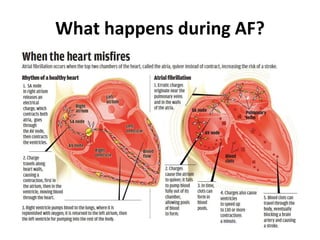
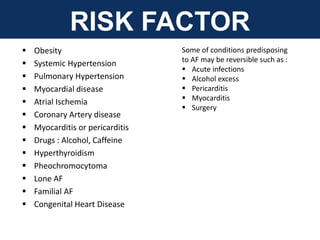
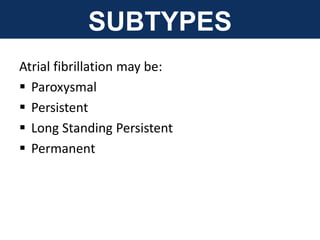
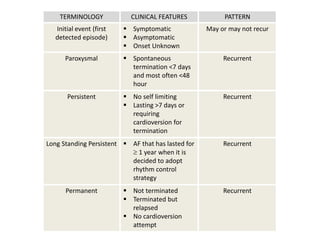
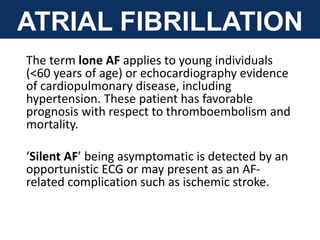
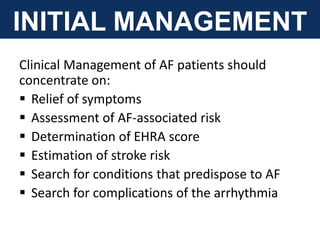
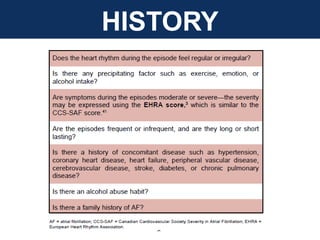
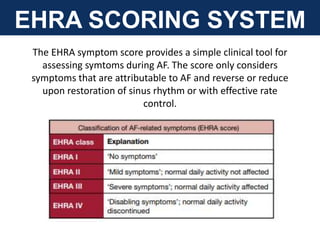
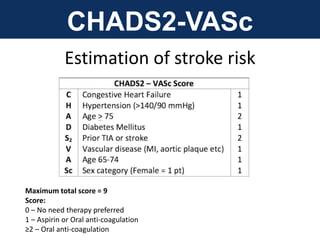
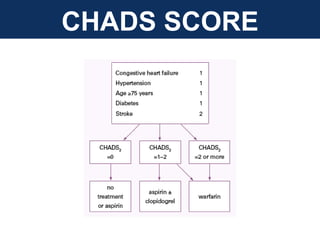
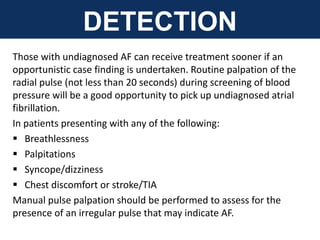
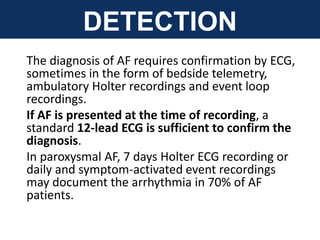
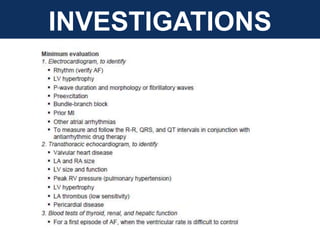
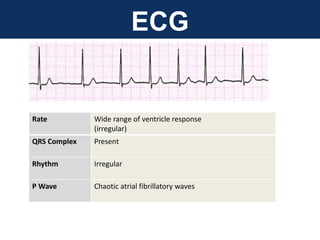
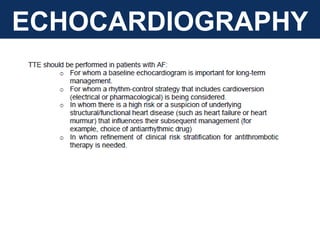
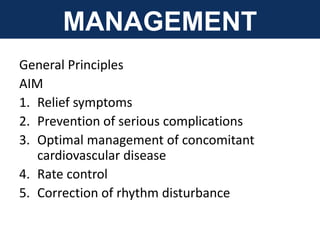
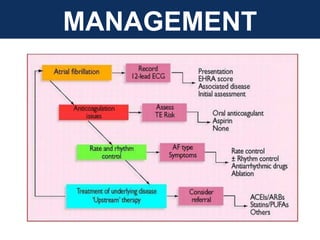
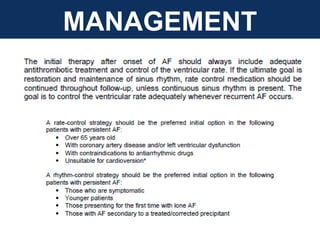
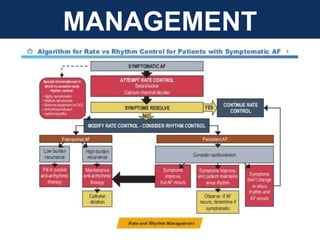
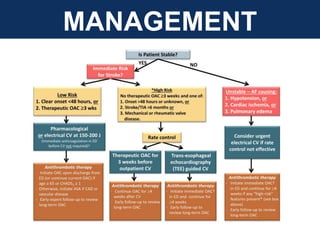
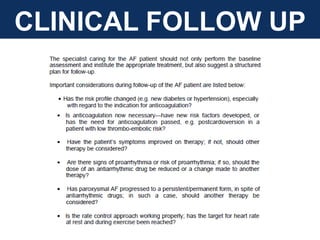
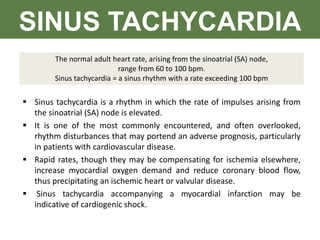
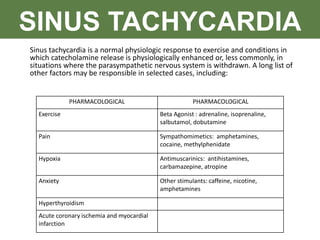
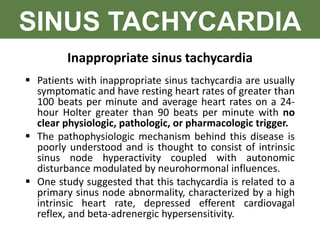
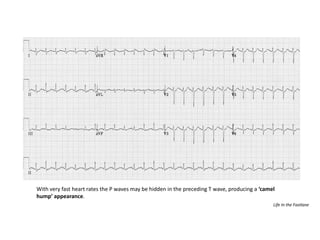
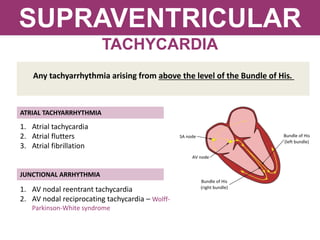
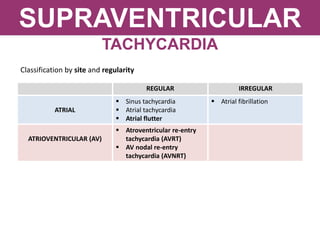
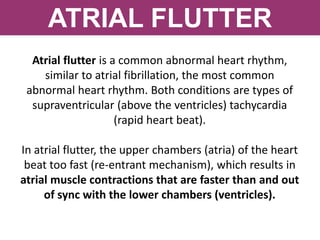
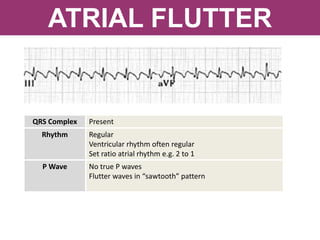
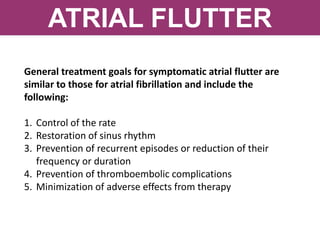
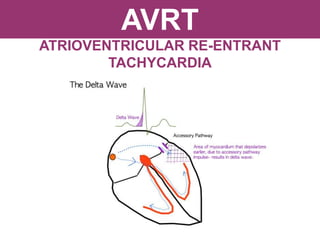
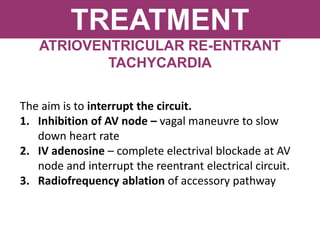
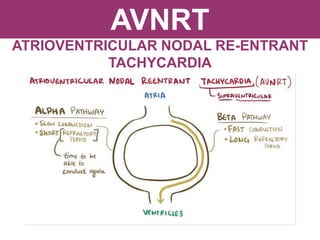
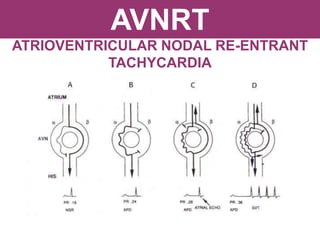
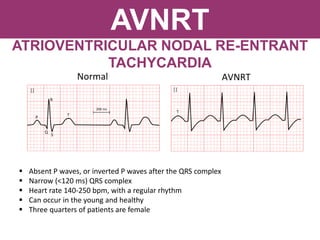
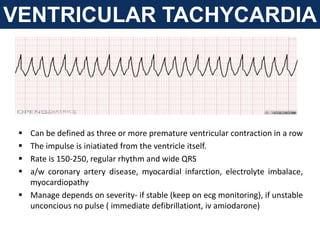
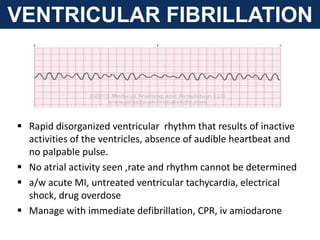
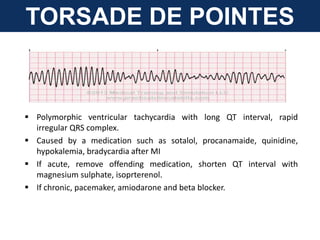
The document provides an extensive overview of cardiac conduction and arrhythmias, detailing their physiology, classification, and pathogenesis. It covers various types of arrhythmias, including bradyarrhythmias and tachyarrhythmias, along with their symptoms, underlying causes, and treatment strategies. Additionally, it discusses the recognition and management of conditions like atrial fibrillation, emphasizing the importance of ECG in diagnosis and risk stratification for stroke and other complications.