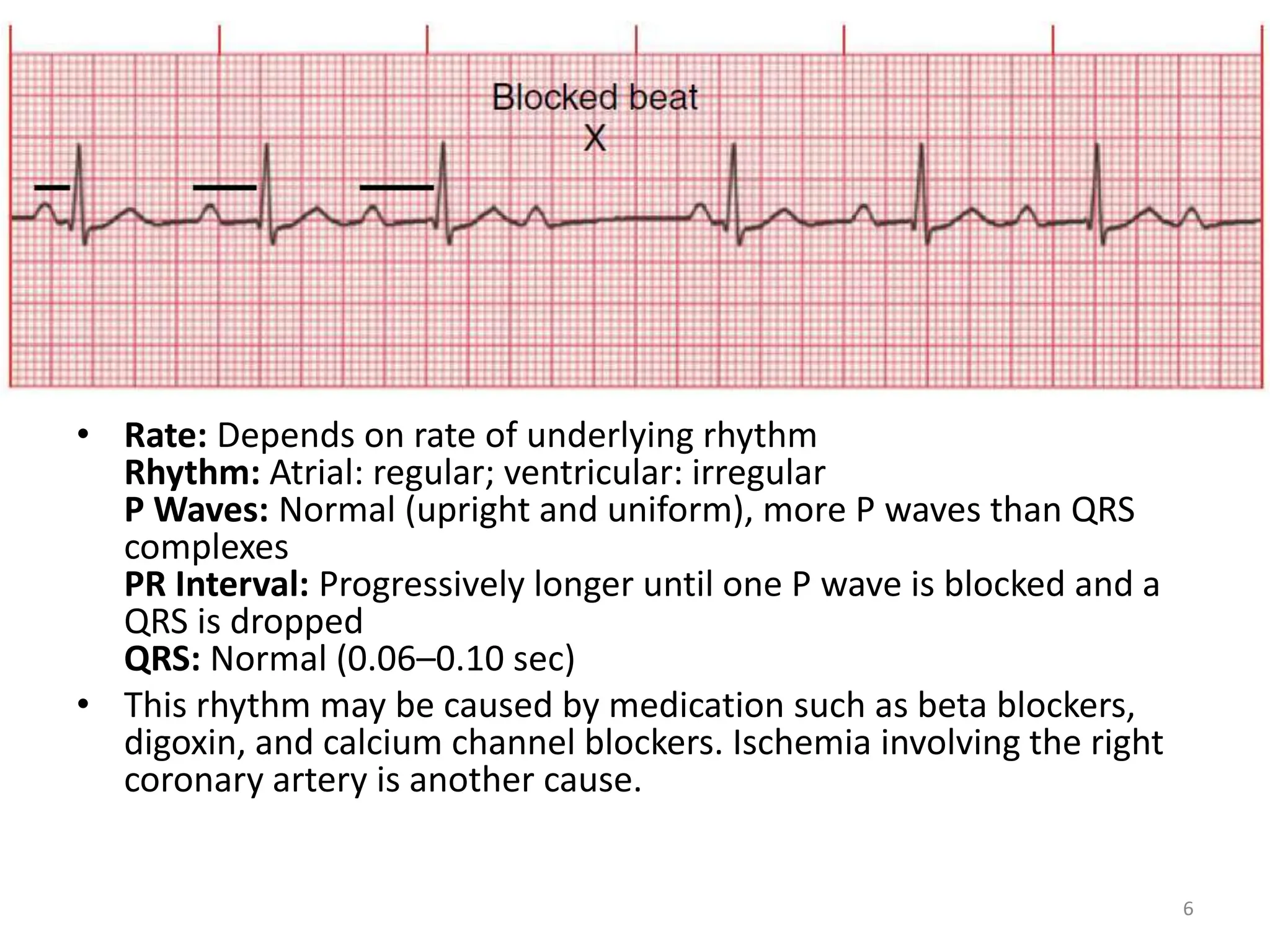
This document discusses different types of atrioventricular (AV) blocks including first, second, and third degree blocks. It provides details on the characteristics, causes, and treatments for each type of block. First degree AV block involves prolonged AV conduction but each impulse is conducted. Second degree blocks involve either progressive PR interval lengthening (Mobitz I) or nonconducted impulses without lengthening (Mobitz II). Third degree or complete heart block results in no conduction between the atria and ventricles. More severe blocks may require pacemaker implantation.