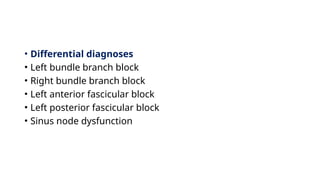
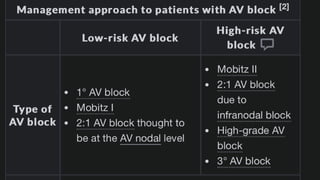
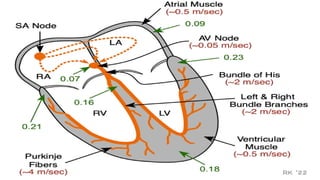
The document provides an extensive overview of atrioventricular (AV) block, including its definition, etiology, pathophysiology, clinical features, and management strategies. It describes various types of AV blocks, factors leading to their development, and the associated risks, highlighting the importance of proper diagnosis and potential pacemaker placement in certain cases. Additionally, it briefly touches on bundle branch blocks and their associated ECG findings.

![2:Neurocardiogenic
A. Increased vagal tone: can be physiological or pathological
A. Healthy individuals with high levels of exercise (e.g., in
professional athletes): most often transient 1° AV
block and Mobitz 1
B. Obstructive sleep apnea
C. During vomiting, suctioning, or intubation [7]](https://image.slidesharecdn.com/avblockpresentation1-250113134333-11333a54/85/AV-Block-presentation-high-yield-1-pptx-7-320.jpg)
![Clinical features
1. Asymptomatic (common): especially with first-degree
and Mobitz type I blocks [2]
2. Clinical features of end-organ hypoperfusion(due
to bradycardia) may be present, including: [9]
1. Fatigue
2. Exercise intolerance
3. Dyspnea
4. Dizziness
5. Syncope](https://image.slidesharecdn.com/avblockpresentation1-250113134333-11333a54/85/AV-Block-presentation-high-yield-1-pptx-11-320.jpg)
![Cont…
• Significant pauses of asystole
• Stokes-Adams attacks [10]
• Sudden losses of consciousness that may occur with
brief prodromal symptoms, e.g., dizziness, or without any warning, usually
lasting a few seconds
• Attacks are caused by ventricular asystole, most commonly due to third-
degree heart block, especially idiopathic paroxysmal AV block.
• Cardiac arrest](https://image.slidesharecdn.com/avblockpresentation1-250113134333-11333a54/85/AV-Block-presentation-high-yield-1-pptx-13-320.jpg)
![Second-degree AV block
1: Mobitz type I (Wenckebach) [2]
• Description
• Progressive lengthening of the PR interval until a beat is dropped, which
means a regular atrial impulse does not reach the ventricles (a normal P
wave is not followed by a QRS complex)
• Mostly regular rhythm separated by short pauses, which may lead
to bradycardia(regularly irregular rhythm)
• Rate of SA node > heart rate
• Risk of progression to complete heart block: typically low, as the
block is most often at the level of the AV node](https://image.slidesharecdn.com/avblockpresentation1-250113134333-11333a54/85/AV-Block-presentation-high-yield-1-pptx-18-320.jpg)


![ Third-degree AV block (complete heart block)
•
• Description
• Third-degree AV block is a complete block with no conduction between the atria and ventricles.
• P waves and QRS complexes have their own regular rhythm but bear no relationship to each other (AV
dissociation).
• Risk of progression to cardiogenic shock or cardiac arrest: High; Sudden onset 3° AV
blockcan result in ventricular asystole, which lasts until an escape rhythm takes over.
• Escape rhythms: can be generated by sites that are usually located near the AV node or
near the bundle of His.
• Ventricular escape rhythm [11]
• A rhythm generated at the level of the bundle of His
• Heart rate 20–40/minute
• Wide QRS complexes
• Junctional escape rhythm [11]
• A rhythm generated at the level of the AV node
• Heart rate 40–60/minute
• Narrow QRS complexes](https://image.slidesharecdn.com/avblockpresentation1-250113134333-11333a54/85/AV-Block-presentation-high-yield-1-pptx-27-320.jpg)