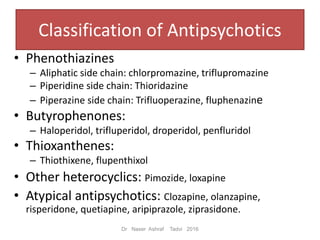
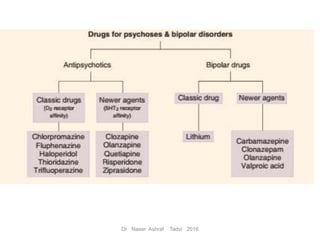
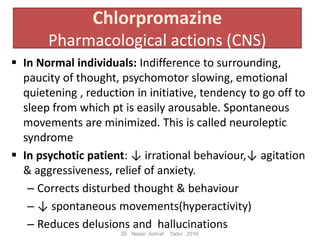
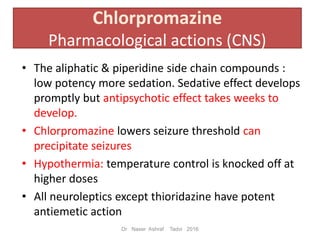
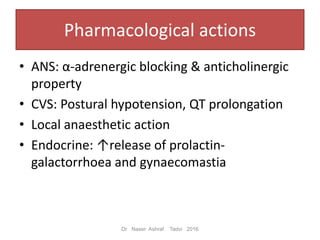
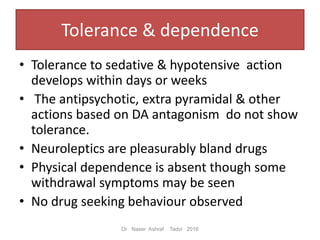
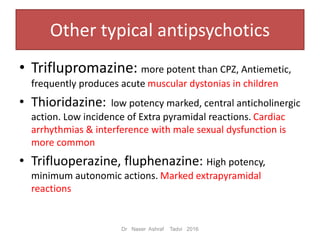
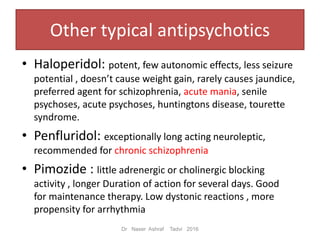
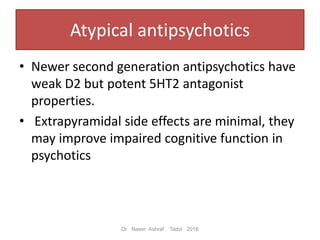
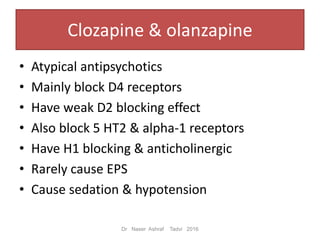
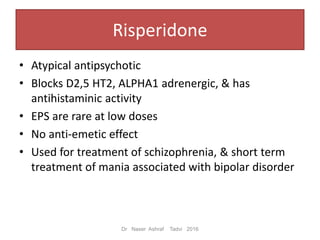
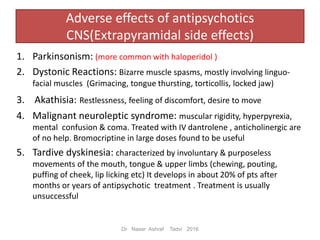
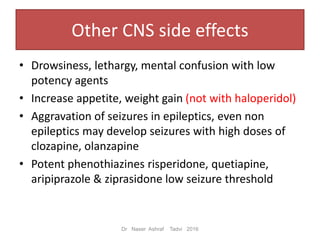
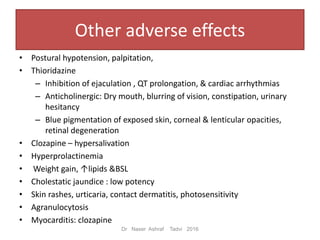
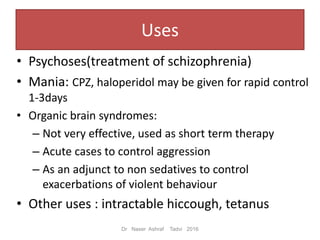
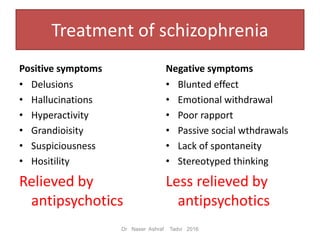
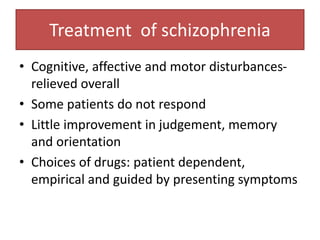
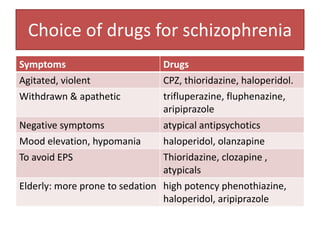
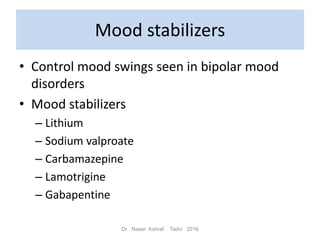
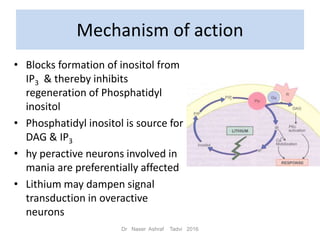
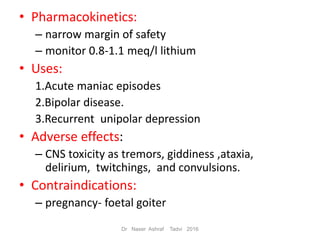
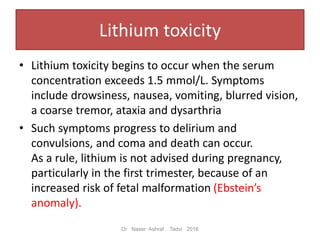
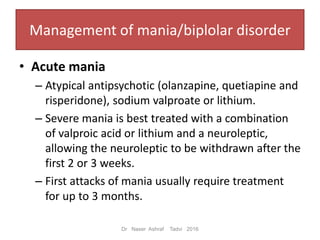
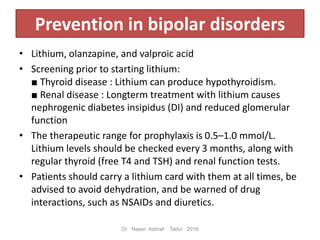
This document discusses antipsychotic and mood stabilizing drugs. It begins by classifying antipsychotics such as phenothiazines, butyrophenones, and atypical antipsychotics. It then describes the mechanism of action, uses, and adverse effects of typical antipsychotics like chlorpromazine and haloperidol. Atypical antipsychotics like clozapine and risperidone are also discussed. The document also covers mood stabilizers lithium and sodium valproate, focusing on lithium's mechanism and use in treating mania and bipolar disorder. Management of schizophrenia, mania, and bipolar disorder is described.